https://www.hrw.org/report/2018/02/05/they-want-docile/how-nursing-homes-united-states-overmedicate-people-dementia
Too many times I’m given too many pills…. [Until they wear off], I can’t even talk. I have a thick tongue when they do that. I ask them not to [give me the antipsychotic drugs]. When I say that, they threaten to remove me from the [nursing] home. They get me so I can’t think. I don’t want anything to make me change the person I am.
—Walter L., an 81-year-old man given antipsychotic drugs in a Texas nursing facility, December 2016.It used to be like a death prison here. We cut our antipsychotics in half in six months. Half our residents were on antipsychotics. Only 10 percent of our residents have a mental illness.
—A director of nursing at a facility in Kansas that succeeded in reducing its rate of antipsychotic drug use, January 2017.
In an average week, nursing facilities in the United States administer antipsychotic drugs to over 179,000 people who do not have diagnoses for which the drugs are approved. The drugs are often given without free and informed consent, which requires a decision based on a discussion of the purpose, risks, benefits, and alternatives to the medical intervention as well as the absence of pressure or coercion in making the decision. Most of these individuals—like most people in nursing homes—have Alzheimer’s disease or another form of dementia. According to US Government Accountability Office (GAO) analysis, facilities often use the drugs to control common symptoms of the disease.
While these symptoms can be distressing for the people who experience them, their families, and nursing facility staff, evidence from clinical trials of the benefits of treating these symptoms with antipsychotic drugs is weak. The US Food and Drug Administration (FDA) never approved them for this use and has warned against its use for these symptoms. Studies find that on average, antipsychotic drugs almost double the risk of death in older people with dementia. When the drugs are administered without informed consent, people are not making the choice to take such a risk.
The drugs’ sedative effect, rather than any anticipated medical benefit, too often drives the high prevalence of use in people with dementia. Antipsychotic drugs alter consciousness and can adversely affect an individual’s ability to interact with others. They can also make it easier for understaffed facilities, with direct care workers inadequately trained in dementia care, to manage the people who live there. In many facilities, inadequate staff numbers and training make it nearly impossible to take an individualized, comprehensive approach to care. Many nursing facilities have staffing levels well below what experts consider the minimum needed to provide appropriate care.
Federal regulations require individuals to be fully informed about their treatment and provide the right to refuse treatment. Some state laws require informed consent prior to the administration of antipsychotic drugs to nursing home residents. Yet nursing facilities often fail to obtain consent or even to make any effort to do so. While all medical interventions should follow from informed consent, it is particularly egregious to administer a drug posing such severe risks and little chance of benefit without it.
Such nonconsensual use and use without an appropriate medical indication are inconsistent with human rights norms. The drugs’ use as a chemical restraint—for staff convenience or to discipline or punish a resident—could constitute abuse under domestic law and cruel, inhuman, and degrading treatment under international law.
The US has domestic and international legal obligations to protect people who live in nursing facilities from the inappropriate use of antipsychotic drugs, among other violations of their rights. These obligations are particularly important as people in nursing facilities are often at heightened risk of neglect and abuse. Many individuals in nursing facilities are physically frail, have cognitive disabilities, and are isolated from their communities. Often, they are unable or not permitted to leave the facility alone. Many depend entirely on the institution’s good faith and have no realistic avenues to help or safety when that good faith is violated.
US authorities, in particular the Centers for Medicare & Medicaid Services (CMS) within the US Department of Health and Human Services, are failing in their duty to protect some of the nation’s most at-risk older people. On paper, nursing home residents have strong legal protections of their rights, but in practice, enforcement is often lacking. Although the federal government has initiated programs to reduce nursing homes’ use of antipsychotic medications and the prevalence of antipsychotic drug use has decreased in recent years, the ongoing forced and medically inappropriate use of antipsychotic drugs continues to violate the rights of vast numbers of residents of nursing facilities. The US government should use its full authority to enforce longstanding laws, including by penalizing noncompliance to a degree sufficient to act as an effective deterrent, to end this practice.
***
LAUNCH MAP
Show More Services
This report documents nursing facilities’ inappropriate use of antipsychotic drugs in older people as well as the administration of the drugs without informed consent, both of which arise primarily from inadequate enforcement of existing laws and regulations. The report is based on visits by Human Rights Watch researchers to 109 nursing facilities, mostly with above-average rates of antipsychotic medication use, between October 2016 and March 2017 in California, Florida, Illinois, Kansas, New York, and Texas; 323 interviews with people living in nursing facilities, their families, nursing facility staff, long-term care and disability experts, officials, advocacy organizations, long-term care ombudsmen, and others; analysis of publicly available data; and a review of regulatory standards, government reports, and academic studies.
This report is especially relevant at this time because the US is aging rapidly. Most of the people in the nursing facilities Human Rights Watch visited are over the age of 65. Older people now account for one in seven Americans, almost 50 million people. The number of older Americans is expected to double by 2060. The number of Americans with Alzheimer’s disease, the most common form of dementia, is expected to increase from 5 million today to 15 million in 2050. The system of long-term care services and supports will have to meet the needs—and respect the rights—of this growing population in coming years.
Social Harm and Health Risks Caused by Antipsychotic Drugs Used Unnecessarily or as Chemical Restraints
The American Psychiatric Association (APA) Practice Guideline on the Use of Antipsychotics to Treat Agitation or Psychosis in Patients with Dementia states that, after eliminating or addressing underlying medical, physical, social, or environmental factors giving rise to manifestations of distress associated with dementia, antipsychotic drugs “can be appropriate” as a means to “minimize the risk of violence, reduce patient distress, improve the patient’s quality of life, and reduce caregiver burden.” However, given the “at best small” potential benefits and the “consistent evidence that antipsychotics are associated with clinically significant adverse effects, including mortality,” it is essential that the drug treatment is only attempted when appropriate.
Nursing facility staff, individuals living in facilities, their families, long-term care advocates, and others told Human Rights Watch that the drugs are not used only as a last resort, after all factors potentially giving rise to a person’s distress have been ruled out, and after nonpharmacologic interventions have been attempted unsuccessfully. Instead, antipsychotic drugs are used sometimes almost by default for the convenience of the facility, including to control people who are difficult to manage.
One facility social worker said that one of the most common “behaviors” leading to antipsychotic drug prescriptions was someone constantly crying out, “help me, help me, help me.” An 87-year-old woman reflected that at her prior facility, which gave her antipsychotic drugs against her will, “they just wanted you to do things just the way they wanted.” A social worker who used to work in a nursing facility said the underlying issue is that “the nursing homes don’t want behaviors. They want docile.” A state surveyor said: “I see way too many people overmedicated…. [Facilities] see it as a cost-effective way to control behaviors.”
Human Rights Watch interviewed people who live in nursing homes and their family members who described the harmful cognitive, social, and emotional consequences of the medications that all too often should never have been administered in the first place: sedation, cognitive decline, fear, and frustration at not being able to communicate. Most or all antipsychotic drugs are associated with sedation and fatigue in people with dementia.
A 62-year-old woman in a nursing facility in Texas who said she was given Seroquel, a common antipsychotic drug, without her knowledge or consent said: “[It] knocks you out. It’s a powerful, powerful drug. I sleep all the time. I have to ask people what the day is.” The daughter of a 75-year-old woman in Kansas said that when the nursing facility began giving her mother an antipsychotic drug, her mother “would just sit there like this. No personality. Just a zombie…. The fight is gone.”
Nursing staff, social workers, long-term care ombudsmen, and state surveyors echoed this perception. One director of nursing said: “You actually see them decline when they’re on an antipsychotic. I think it’s sadder than watching someone with dementia decline.”
Lack of Informed Consent Prior to Antipsychotic Medication Administration
The use of antipsychotic drugs to control people without their knowledge or against their will in nonemergency situations violates international human rights. The practicalities of obtaining consent from an older person with dementia can be fraught. However, in many of the cases Human Rights Watch documented, nursing facilities made no effort to obtain meaningful, informed consent from the individual or a health proxy before administering the medications in cases where it clearly would have been possible to do so.
Our research suggests that in many other cases, facilities that purport to seek consent fail to provide sufficient information for consent to be informed; pressure individuals to give consent; or fail to have a free and informed consent procedure and documentation system in place. Under international human rights law, in the absence of free and informed consent, a nonemergency medical intervention that is not necessary to address a life-threatening condition is forced treatment.
One former nursing facility administrator explained:
The facility usually gets informed consent like this: they call you up. They say, “X, Y, and Z is happening with your mom. This is going to help her.” Black box warning (the government’s strongest warning to draw attention to serious or life-threatening risks of a prescription drug)? “It’s best just not to read that.” The risks? They gloss over them. They say, “That only happens once in a while, and we’ll look for problems.” We sell it. And, by the way, we already started them on it.
A current director of nursing admitted, “We are supposed to be doing informed consent. It’s on the agenda. But really antipsychotics are a go-to thing. ‘Give ‘em some Risperdal and Seroquel.’ We tell the family as we’re processing the order. The family is notified.” The daughter of a woman in a nursing facility described having consented to antipsychotic drugs for her mother without understanding the risks: “I had no idea, not at all, that the drugs were dangerous. I had no idea…. I’m guessing most people have no idea.”
A detailed examination of the question of legal capacity—the right to exercise one’s own rights and to make decisions on one’s own behalf—is outside the scope of this report. Because many people living in nursing facilities have dementia and other progressive conditions that affect their cognitive ability, it is a highly complex question how medical and other decisions concerning their care should be made in a rights-respecting manner. In US nursing facilities, substituted decision-making—where a family member or other third party, whether voluntarily designated in advance or not, makes decisions on an individual’s behalf—is common.
Government Obligations
In 2012, CMS created the National Partnership to Improve Dementia Care in Nursing Homes, in recognition of the unacceptably high prevalence of antipsychotic drug use. While the initiative—which set targets for the industry to reduce antipsychotic drug rates—may have contributed to the reduction of the use of antipsychotic medications over the last six years, it cannot substitute for the effective regulation of nursing homes, including by ensuring that facilities face meaningful sanctions for noncompliance with mandatory standards. Our research found that CMS is not using its full authority to address this issue. Recently, CMS is in fact moving in the opposite direction, limiting the severity of financial penalties and the regulatory standards with which facilities must comply.
CMS and the state agencies with which it contracts to enforce federal regulations are not meeting their obligation to protect people from the nonconsensual, inappropriate use of antipsychotic drugs. Human Rights Watch identified several key areas of concern:
- Failure to adequately enforce the right to be fully informed and to refuse treatment or to require free and informed consent requirement. The Nursing Home Reform Act of 1987 grants residents the right “to be fully informed in advance about care and treatment,” to participate in care planning, and to refuse treatment without penalty. If it were enforced fully, these protections would not differ substantially from the right to free and informed consent. However, without adequate enforcement, current practice falls far short of this protection.
- Lack of minimum staffing regulations. Adequate numbers of sufficiently competent staff are at the crux of nursing facility care. Yet government regulations do not set a minimum staffing requirement for nursing facilities, instead requiring that facilities determine for themselves what amounts to “sufficient” and “competent” staff for their residents. While experts put minimum adequate nursing staffing time at 4.1 to 4.8 hours per resident per day, most facilities self-reported to the government providing less than that; almost one thousand facilities self-reported providing less than three hours of staff time per day.
- Weak enforcement of federal regulations specifically banning chemical restraints and unnecessary drugs. Federal regulations prohibit chemical restraints—drugs used for the convenience of staff or to discipline residents without a medical purpose—and unnecessary drugs: a technical term meaning drugs used without adequate clinical indication, monitoring, or tapering. The regulations also provide for the right to refuse treatment. However, federal and state enforcement of these regulations is so weak that the drugs are routinely misused without significant penalty. Almost all antipsychotic drug-related deficiency citations in recent years have been determined to be at the level of causing “no actual harm,” curtailing the applicability and severity of financial sanctions.
With such vast numbers of nursing facility residents still getting antipsychotic drugs that many do not need, do not want, and that put their lives and quality of life at risk, federal and state governments need to do more to ensure that the rights of residents are adequately protected. An industry entrusted to provide care—and paid billions of public and private dollars to do so—cannot justify compounding the vulnerabilities, challenges, and loss that people often experience with dementia and institutionalization.
BACK TO TOP
Related Content
-
- February 5, 2018 News Release
Key Recommendations
Federal and state government agencies should take steps to end the inappropriate and nonconsensual use of antipsychotic medications in nursing facilities. In particular, the Centers for Medicare & Medicaid Services (CMS) and other government agencies should:
- End the inappropriate use of antipsychotic drugs in older people with dementia in nursing facilities, including many instances where they are administered without free and informed consent; used as chemical restraints; or where their use qualifies as an “unnecessary drug.” CMS and state agencies should use the regulatory and enforcement tools at their disposable to ensure that routine violations of regulations that help to safeguard individuals’ human rights cease.
- Require nursing facilities and residents’ physicians to seek free and informed consent prior to the administration of antipsychotic medications to nursing facility residents. Federal regulations providing for the right to be fully informed and to refuse treatment—as well as state laws that provide for informed consent—should be enforced more effectively. The establishment in the federal regulations of a right to informed consent may improve protection in practice by clarifying the right’s content and underscoring its significance. Congress and CMS should require that consent be documented and revisited as appropriate.
- Ensure nurse staffing numbers and training levels are adequate. CMS should establish minimum nurse staffing levels for facilities or undertake other effective measures to address understaffing, inadequate training, and high turnover rates in many nursing facilities. Implementation of the payroll-based staffing data collection system, as required by the Affordable Care Act, should be completed, particularly with regard to nursing staff who provide direct resident care. This includes public reporting of staff-to-resident hours of care per day and turnover and retention rates in each nursing home certified by Medicare and Medicaid.
- Strengthen enforcement on particular subjects linked to the inappropriate use of antipsychotic drugs, including care planning requirements and transfer and discharge rights. CMS should improve inspection and penalty guidance and enforcement practices related to antipsychotic drugs. Surveyors should follow CMS guidance indicating that many inappropriate uses of antipsychotic drugs amount to Level 3 or 4—actual harm and immediate jeopardy—severity of violations.
BACK TO TOP
Methodology
This report focuses on the inappropriate use of antipsychotic drugs among older people, primarily with dementia, in nursing facilities across the US. Many older people who live in nursing facilities or reside there temporarily are at risk of suffering from this abuse. They rely on the government’s enforcement of federal regulations to protect their rights, including to be free from unnecessary drugs, drug treatment to which they object, and sedating drugs administered for the convenience of facility staff. Human Rights Watch found that enforcement is inadequate to deter the misuse of antipsychotic drugs.
This topic was chosen because of the paradox that misuse of the drugs has been well-documented for decades, prohibited by law, and yet persists as a pervasive, serious problem. The amount of publicly available data on nursing homes and antipsychotic drugs specifically made it feasible to conduct the research. The project was also chosen to attempt to amplify the voice and highlight the circumstances of some of the most isolated individuals: not only by living in nursing homes or having dementia, but also by being under the influence of the psychotropic medication.
The report is based on interviews with 323 people in New York, Texas, Kansas, Illinois, California, and Florida between October 2016 and March 2017. Additional interviews were conducted over the phone from September 2016 to April 2017. In addition, Human Rights Watch consulted secondary sources, conducted significant background research, and analyzed copious amounts of data.
These six states were selected for multiple reasons. California and Texas have the highest number of nursing facilities, with 1,219 and 1,212 respectively in 2014. California, Florida, Illinois, New York, and Texas have among the highest numbers of nursing facility residents of any state. Excluding facilities where less than half of the residents are over age 65, Texas and New York lead all states in terms of the number of nursing home residents taking antipsychotic drugs without an exclusionary diagnosis of schizophrenia, Huntington’s disease, or Tourette syndrome. Kansas, Texas, and Illinois have some of the highest proportions of residents on antipsychotic drugs. More detailed data on these states and their rankings nationally can be found in Appendix 3. Most of these states were also chosenbased on their strong citizen advocacy organizations working on nursing facility reform and resident rights protection and their long-term care ombudsman programs.
In the six states, Human Rights Watch interviewed 74 people between the ages of 37 and 93 who live in nursing facilities, including 15 under the age of 65. All of the individuals in nursing facilities had cognitive, psychosocial, and/or physical disabilities. Almost all of the individuals were in facilities with high rates of antipsychotic drug use; in many cases, they or someone who knows them told Human Rights Watch that they currently or previously took antipsychotic drugs. However, not all interviewees claimed to take antipsychotic drugs, and it was not possible to view the medical records of the majority of interviewees.
We interviewed 36 family members of residents, 20 long-term care ombudsmen, 18 advocates including attorneys, 10 state and federal government officials, 90 facility administrators, nursing, and social services staff, and six medical professionals such as pharmacists, psychologists, psychiatrists, and doctors. We have omitted people’s names or used pseudonyms where names or other identifying information may compromise the privacy of individuals or invite possible reprisals.
Human Rights Watch also interviewed 69 experts, including lawyers, academic researchers, professors, journalists, doctors (in addition to those interviewed associated with nursing facilities or nursing facility residents mentioned above), government officials, and advocates. Human Rights Watch sent letters to CMS, the American Health Care Association (AHCA), and LeadingAge—the government agency that oversees the nursing facility industry, the for-profit trade association, and the nonprofit trade association, respectively—with questions regarding this report’s findings. We received responses from AHCA and LeadingAge (see Appendices 6 and 7). We did not receive a response from CMS at time of writing.
Human Rights Watch visited 109 facilities. In 17 of the 109 facilities, we were not allowed to conduct research. Of the remaining 92, sometimes our entry was with explicit permission of the facility, sometimes with permission of the person we were visiting, and sometimes without permission of the facility but without objection. In some cases, we talked to staff only and not residents.
Two of the 109 facilities were in New York, 25 in Texas, 20 in Kansas, 16 in Illinois, 23 in California, and 23 in Florida. One of the 109 has since closed. All facilities were skilled nursing facilities or nursing facilities rather than assisted living facilities, and all received some combination of payment through Medicare, Medicaid, private insurance, and private pay. The US Department of Veterans Affairs operates community living centers, nursing homes, and state veterans’ homes across the country as well, as part of the Veterans Health Administration; they are regulated differently and outside the scope of this project. Facilities were selected based on publicly available data on the average percentage of residents without an exclusionary diagnosis given at least one antipsychotic medication in the last quarter.
We primarily visited facilities with a majority population over the age of 65. As of 2010, 16 percent of the nation’s nursing home population was between the ages of 31 and 64. Younger people live in nursing facilities for a variety of reasons. However, nursing homes with majorities of younger people and high rates of antipsychotic drug use tend to have greater concentrations of people with psychosocial disabilities. While the administration of antipsychotic drugs may be inappropriate despite psychiatric diagnoses for which the drugs are approved, the root of the rights violations may be distinct, and this report was limited to the demographic of older people, often with dementia.
Of the 109 facilities visited, 79 facilities (72 percent) were for-profit and corporate owned; five (5 percent) were for-profit and individually owned; five (5 percent) were for-profit and part of a partnership government hospital district; 16 facilities (15 percent) were nonprofit and corporate owned; and one facility (1 percent) was nonprofit and church related.
Researchers were refused admission or asked to leave shortly after arriving in 24 facilities. In some cases, administrators had notice of our interest in visiting and refused to meet or allow us to speak with residents who might wish to speak with us. In other cases, facilities did not have notice and requested that we return at another time.
Whenever possible, Human Rights Watch spoke directly with people who live in nursing facilities. In some cases, nursing facility administrators, directors of nursing, directors of social services, or business or admissions officers refused our request to speak with residents. Some facilities claimed that no resident was their own “responsible party” and that they thus could not consent to an interview.
Where access to residents was not blocked, Human Rights Watch sought to interview residents and staff in private so that they could speak openly without fear of potential retaliation. In some facilities, finding locations that afforded sufficient privacy was difficult. As a result, in some cases, with the interviewee’s permission, we conducted interviews in rooms where the interviewee’s roommate was asleep or watching television. In other cases, we conducted interviews in an activity room or at the end of a hallway that was out of ear shot of other people, but not fully secluded.
Human Rights Watch asked interviewees questions on a wide range of issues, including use of antipsychotic medicines; quality of care; quality of life; demographics of the facility residents; access to health care and rehabilitative services; respect for free and informed consent; autonomy; privacy; visitation; and discharge rights.
Interviews were conducted in English or Spanish. Human Rights Watch obtained the consent of each interviewee; explained the aim of the research; how information collected would be used; and informed them that they could discontinue the interview at any time and could decline to answer questions without consequence. Human Rights Watch provided no personal service or benefit and informed interviewees that their participation was voluntary and confidential.
Finding and interviewing people on antipsychotic drugs is difficult for a number of reasons. First, many are unaware because they were never informed, or are unable to recall, that they are on these medications. Facility staff sometimes do not inform the individuals concerned—or their relatives, the legal representative in some cases—that they are being given antipsychotic drugs.
Second, the effect of the medications can make it difficult to respond to interview questions, and the drugs often make people drowsy.
Third, most people in nursing homes have dementia or other cognitive disability. Additionally, most people given antipsychotic drugs without an “exclusionary diagnosis”—schizophrenia, Huntington’s disease, or Tourette syndrome, the most clear-cut and common conditions for which antipsychotic drugs are approved—have dementia, which affects memory and the ability to express oneself understandably.
Fourth, privacy concerns make determining who is receiving the medications difficult.
Fifth, nursing facility staff often do not consider residents to be their own “responsible party”—a term of art frequently used in an overly broad manner to indicate who can exercise a person’s rights. In many cases, facility staff decided on behalf of all residents that Human Rights Watch could not interact with them, often justifying that decision by invoking the need to protect residents.
Informed consent and legal capacity—the right to exercise one’s rights and to make decisions—are critical human rights linked inextricably with the question of appropriate antipsychotic drug use. The administration of psychoactive medication may violate a person’s rights if it is not administered with informed consent. Legal capacity controls whose consent is necessary and valid. However, a comprehensive analysis of consent and legal capacity is beyond the scope of this report. The report focuses on violations of the right to informed consent in cases where it was clearly possible for the facility to seek it, either because a person lacked any severe cognitive disability or because the person had voluntarily designated a proxy to act on their behalf.
Because of significant practical challenges, the residents interviewed do not reflect the most isolated and at-risk people in nursing facilities: people who are on their own, without family or friend visiting or communicating with the facility staff, and who have significant cognitive disabilities that impair their ability to communicate or advocate on their own behalf. Compounding the aforementioned challenges in interviewing residents, for these “unbefriended” or “unrepresented” individuals, there is the additional barrier of not having any intermediary person to identify and connect Human Rights Watch researchers to the person living in the nursing facility.
It is these individuals with severe cognitive disabilities and without someone to assist their communication or decision-making whose rights to legal capacity and informed consent are at the greatest risk of violation. However, they are also the individuals whom it is hardest to access to inquire about an interview and hardest to interview. As a result, the rights violations documented in this report reflect those experienced by people in nursing homes either able to more easily communicate with Human Rights Watch researchers or those experienced by people with family or friends involved in their care.
This report does not analyze nonconsensual use of antipsychotics in nursing facilities on persons who have a diagnosis for which antipsychotics have been approved. Rather, it focuses on the use of these drugs on people with dementia. This report also does not address the process in which people are placed in nursing homes. These issues are complex and go beyond the scope of this report.
Human Rights Watch relied upon several data sets for the quantitative analysis involved in this report, including one provided by Nursing Home Compare. This website, maintained by CMS, provides facility- and state-level data based on the Minimum Data Set (MDS), a federally mandated national database of periodic, individual, clinical, comprehensive assessments of all residents in Medicare and Medicaid certified nursing homes. Nursing facilities submit electronically the MDS information. Nursing Home Compare includes other self-reported and governmental surveyor-reported data for all facilities in the country certified to receive payment from Medicare and Medicaid, which is almost all facilities nationwide.
Despite the volume of publicly available data on the use of antipsychotic drugs in nursing facilities, a number of significant challenges arose in conducting quantitative analyses. First, it is not possible to determine from a single publicly available data set the proportion of all individuals with dementia in nursing facilities without a psychiatric or neurological diagnosis for which an antipsychotic drug is clinically indicated that takes antipsychotic medication. Second, a significant amount of the data on nursing homes is self-reported by those facilities, some of which could be inaccurate and as such may influence the results of statistical tests that Human Rights Watch ran.
Nonetheless, through quantitative data analysis, Human Rights Watch was able to estimate the total numbers of people who receive antipsychotic drugs, live in nursing facilities with a majority population over the age of 65, and do not have an exclusionary diagnosis. (Age 65 is a rough cut-off point to exclude people who are younger and given antipsychotic drugs, appropriately or not, since this research was focused on older people.) We also analyzed antipsychotic drug-related deficiency citations, which are federal and state government inspectors’ findings of facilities’ noncompliance with the federal regulations that establish minimum health and safety standards for the industry. A detailed description of the methodology used can be found in Appendix 4.
BACK TO TOP
I. Background
Long-Term Care in the US
The population of the US is growing older. Between 2005 and 2015, the country’s population aged 65 and over increased by 30 percent. Older people now account for one in seven Americans: almost 50 million people, over 26 million women and over 21 million men.[1] By 2060, the number of older Americans (age 65 and older) is expected to double to almost 100 million, or one in four Americans.[2] The population aged 85 and over is growing particularly rapidly and is expected to triple by 2050.[3] The US population will include so many older people in the coming decades because of the baby boom generation is aging while fertility rates continue to decline and life expectancy rates have increased.[4]
As the older population increases, more people will experience age-related disabilities, and dementia in particular.[5] Today, over 5 million Americans have Alzheimer’s disease or another form of dementia, involving the loss of cognitive abilities, memory, and language.[6]By 2050, as many as 16 million Americans could have Alzheimer’s disease; currently, one person in the United States develops the condition almost every minute of every day.[7]
With the growth in older populations and the increases in debilitating conditions such as dementia, the need for long-term care and support services will grow rapidly. Although some forms of dementia have earlier onset, the disease is associated with older age: increasing age is the “greatest known risk factor” for Alzheimer’s disease.[8] Experts estimate that approximately 70 percent of people aged 65 and over will require long-term services and support, ranging from limited support in their own homes and communities to around-the-clock care in institutional settings.[9]
In the US, older people receive long-term care in a variety of settings: at home, in institutional facilities, and in in-between settings like retirement communities, senior housing, assisted living facilities, and board and care homes. Skilled nursing facilities (which provides short-term rehabilitation) and nursing facilities (for long-term care) provide certified and regulated services to people with significant healthcare and assistance needs.
Of the 6 million older people receiving long-term care, about 4 million receive care from a home health agency at home.[10] About 1.2 million people aged 65 and over lived in 15,600 nursing facilities in 2014, and almost 780,000 people lived in other residential care communities.[11] The proportion of people living in institutional settings increases with age because care needs become more intensive.[12]
Other institutional care settings like assisted living are non-medical and provide minimal supervision. Medicare and Medicaid do not pay for assisted living in most cases.[13] Medicare is the primary provider of health insurance to people aged 65 and older in the United States. It includes four parts: Parts A, B, C, and D, covering hospital insurance (including the first 100, rehabilitative days in a skilled nursing facility); medical insurance (such as doctors, outpatient care, medical equipment, and preventive services); private companies’ health plans (Medicare Advantage); and prescription drugs (including long-stay nursing facility residents’ drug prescriptions), respectively.[14]
Medicaid, which is the primary public health insurance program for people with low income in the US and is jointly administered by the federal government and the states, is the primary payer for long-term care, accounting for 51 percent of the nursing home industry’s expenditures.[15] Consequently, to receive institutional long-term care outside of a nursing facility requires significant private resources, estimated at over US$3,000 per month.[16]
The total cost of long-term care varies by context. In 2015, the median annual cost of living in a nursing facility was over $90,000, roughly twice the cost of having a home health aide and five times the cost of an adult day health care program (almost $18,000).[17] Long-term care costs vary significantly by state. For example, a semi-private skilled nursing home room in the most expensive states (Alaska, Connecticut, and Massachusetts) costs almost three times as much as in the least expensive states (Texas, Missouri, and Louisiana), $143,000–$168,000 compared to $56,000–$61,000 annually. Moreover, home health aides in the most expensive states (Massachusetts, Alaska, and New Jersey) cost almost twice as much as in the least expensive states (Alabama, Louisiana, and West Virginia), $28–$31 versus $17–$19 hourly.[18] In 2013, approximately half of Medicare beneficiaries, which include older people and younger people with disabilities, earned less than $23,500 per year.[19]
Despite the common perception that Medicare is for older people and Medicaid is for the poor, many people in the middle class in nursing facilities depend on Medicaid. Many people who saved for assisted living or other non-nursing facility care spend down their savings rapidly. In 2012, paying privately for the median cost of a nursing home ($81,030) would cost 252 percent of the median household income ($34,381) for people aged 65 and up.[20] One in three people turning 65 may require care from a nursing facility at some point in their life, and three-quarters of long-term nursing facility residents will be covered by Medicaid at some point.[21]
The US Nursing Facility Industry
Seventy percent of nursing facilities in the US—about 11,000—are owned by for-profit companies, and almost 25 percent are nonprofit.[22] About 6 percent are publicly owned, most of which (46 percent) are owned by counties, followed by hospital districts (21 percent), states (14 percent), city-county (9 percent), city (8 percent), and the federal government (1 percent).[23] In 2014, almost three in five nursing facilities were part of a chain, meaning they were owned by an entity that owns multiple facilities.[24] Private equity firms own about 12 percent of all nursing facilities (18 percent of for-profit ones).[25] Ten chains own the facilities in which 14 percent of the nation’s residents live, the largest concentration.[26]
In 2015, the nursing facility industry, assisted living, and other types of long-term care recorded annual revenues of $156.8 billion, 41 percent of which came from Medicaid and 21 percent from Medicare.[27] Medicare and Medicaid have provided the financial foundation of the nursing facility industry since their creation.[28]
The federal government regulates the nursing facility industry through the Nursing Home Reform Act of 1987, requiring facilities to meet certain standards to be certified and paid by Medicare and Medicaid.[29] CMS contracts with state agencies to certify facilities and to ensure “substantial compliance” with minimum health and safety requirements.[30]
In subsequent sections, this report describes the inappropriate use of antipsychotic drugs in older people with dementia in US nursing facilities—including use without valid medical reason; for the convenience of staff; inconsistent with federal regulatory requirements; and without informed consent. The report discusses the inadequacy of federal regulations, enforcement, and access to private remedies for harm.
This background section describing the long-term care system provides the context to understand—and highlights the salience of—facilities’ abuses and governmental shortcomings. The population is aging, and long-term care services and supports, including nursing homes, are more likely to be necessary as age-related disabilities rise. It is not only the poor who end up in nursing facilities but many people in the middle class: people who never had and never anticipated relying on Medicaid. Dementia—a risk factor for being given antipsychotic drugs in nursing homes inappropriately, until the government enforces protections against such abuse more effectively—affects people across income, gender, and race.
The industry’s reliance on Medicare and Medicaid described in this section, as well as the breakdown in the industry by ownership status, with the prevalence of chain ownership, relate to regulatory and enforcement concerns. As noted, facilities are required to comply with certain standards of care to receive certification and payment from Medicare and Medicaid: these health insurance programs are the government’s basis for regulating facilities.
BACK TO TOP
II. The Risks and Harms of Antipsychotic Medications on People with Dementia in Nursing Facilities
I would just shut off and not say anything. [It] was a very traumatic time.
—Madeline C., an 86-year-old woman at a nursing facility in Illinois describing being on antipsychotic medications, February 2017.[31]
Antipsychotic drugs were originally developed to treat schizophrenia. The first generation—so-called “conventional” antipsychotics, such as Haldol (haloperidol)—was developed in the 1950s, and a second generation—called “atypical” antipsychotics, such as Seroquel (quetiapine)—was developed in the 1980s.[32] The US Food and Drug Administration (FDA) has approved some of these medicines for treatment of other conditions since then, such as Tourette syndrome and bipolar disorder.[33] The FDA has not approved antipsychotic drugs for treating symptoms of dementia.
Antipsychotic medications are one of several classes of psychotropic drugs affecting the central nervous system. Psychotropic drugs include anti-anxiety medications, anti-depressants, hypnotics, anxiolytics and sedatives like benzodiazepines (e.g., Xanax, Ativan, Valium, Klonopin), anticonvulsants, and mood stabilizers (e.g., Depakote or lithium, often used for bipolar disorder), some of which have comparable effects to antipsychotic drugs and all of which are used prevalently in nursing facilities.[34] (CMS has expressed concern that, as the use of antipsychotic drugs in people with dementia is discouraged as inappropriate, these other classes of medications should not replace them.[35]) Other types of psychotropic drugs, such as anti-anxiety drugs, can have similar sedating properties and cause adverse effects if used inappropriately. In revising federal regulations in 2016, CMS wrote:
Expanding the requirements for antipsychotic drugs to psychotropic drugs will expand protections for residents prescribed drugs that have an increased potential for being prescribed inappropriately or for reasons other than the resident’s benefit, such as for the purpose of a chemical restraint.[36]
Antipsychotic medicines are widely used off-label, that is, for indications or purposes for which the FDA has not approved them. Off-label use of medication is both common and legal. However, the problem with the use of antipsychotic drug in older people with dementia is beyond the issue of legality. As the FDA states in the boxed warning manufacturers must include on conventional and atypical antipsychotic drug labels, elderly patients with “dementia-related psychosis” treated with antipsychotic drugs are at an increased risk of death.[37] It is uncommon for the FDA to require a boxed warning regarding a never-approved use of a drug. Neither off-label use nor the use warned against in boxed warnings affects Medicare coverage of the drug.[38]
The boxed warning on antipsychotic drugs for use in older people with dementia is based on findings that the drugs increase the risk of death in older people with dementia.[39]
| Quetiapine Fumarate (SEROQUEL XR®)Extended-release tablets200mg*, once dailyWARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSISElderly patients with dementia-related psychosis treated with atypical antipsychotic drugs are at an increased risk of death compared to placebo. Analyses of seventeen placebo-controlled trials . . . in these patients revealed a risk of death in the drug-treated patients of between 1.6 and 1.7 times that seen in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. [This drug] is not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions (5.1)].[40] |
| A Mock-Up of the Boxed Warning on Antipsychotic Drugs. |
Aside from raising the risk of death, the drugs’ side effects include severe nervous system problems; neuroleptic malignant syndrome (a life-threatening reaction associated with severe muscular rigidity, fever, and altered mental status); tardive dyskinesia (characterized by stiff, jerking movements that may be permanent once they start and whose likelihood of onset increases the longer antipsychotic drugs are taken); high blood sugar and diabetes; and low blood pressure, which causes dizziness and fainting.[41] Other side effects include increased mortality, cerebrovascular events (stroke), cardiovascular effects, blood clots, central and autonomic nervous system problems, visual disturbances, metabolic effects, extrapyramidal symptoms, fall risk and hip fracture, irreversible cognitive decompensation, and pneumonia.[42]
In the context of nursing facilities, the most common use of these medications is in older people with dementia for the “behavioral and psychological symptoms of the disease.”[43] A 2012 Office of Inspector General investigation found that Medicare processed 1.4 million claims for atypical antipsychotic drugs from nursing facilities in 2007. Older people with dementia accounted for 88 percent of the 1.4 million claims.[44] Only 4.7 percent of these claims were for medications that were not used in older people with dementia and were not used for an off-label use. In other words, they were used for someone with schizophrenia or another psychiatric or neurological condition for which the drugs are approved.[45]
The medical reason for prescribing antipsychotic drugs to people with dementia, usually as a last resort, is that dementia is often accompanied by irritability, agitation, aggression, hallucinations, delusions, wandering, disinhibition, anxiety, and depression—what some medical professionals call “behavioral and psychological symptoms of dementia.”[46]
Some studies find that a majority of people with dementia will develop at least one of these symptoms and that individuals in nursing facilities tend to have more severe symptoms than people in other care settings.[47] These symptoms can be distressing and dangerous to the individuals experiencing them and to those around them, including family and caregivers.[48] Nursing facility staff that administer antipsychotic drugs to older people inappropriately but who are not administering them intentionally for staff convenience often appear to believe that the drugs are the best or only treatment option for someone seemingly in distress.
Dementia-related symptoms may result from “underlying neurochemical changes,” changes in the body’s nervous system, associated with dementia or from an external or underlying situation such as pain or personal needs.[49] Pain is often underreported in people with dementia.[50] Unlike schizophrenia and other psychiatric conditions, the “behaviors” of people with dementia often arise from feelings of loneliness, boredom, depression, anxiety, sun-downing (increased agitation or distress in early evening), apathy, distrust of new caregivers, hunger, dehydration, impairment of the brain’s executive function, grief, noise stress, and delirium.[51]
In addition to unmet physical needs, symptoms may be a “response to environmental triggers,” such as being ignored unless a person screams (which inadvertently reinforces the “behavior” of screaming); alternatively, symptoms may be “consequences of a mismatch between the environment and patients’ abilities to process and act upon cues, expectations and demands.”[52] An example of such a distressing mismatch is “resisting care” when expected to be showered if it frightens a person by association with a prior fall. In its revised guidance that intended to go into effect in November 2017, CMS states:
Behavioral or psychological expressions are occasionally related to the brain disease in dementia; however, they may also be caused or exacerbated by environmental triggers. Such expressions or indications of distress often represent a person’s attempt to communicate an unmet need, discomfort, or thoughts that they can no longer articulate.[53]
Experts agree on the importance of attempting nonpharmacologic interventions with individuals with dementia-related symptoms; federal regulations also require such interventions unless clinically contraindicated (when the intervention should not be used due to adverse effects).[54] These interventions follow these steps: evaluating and understanding the origin of the “behavior”; ruling out underlying physical illness, infection, or needs; addressing any underlying dementia-related or environmental issue; and re-evaluating the care plan based on its effectiveness.[55]
Examples of nonpharmacologic interventions include:
- Reducing boredom, pain, loneliness, and similar experiences by changing a person’s activities, surroundings, opportunities, and access to relationships;
- Creating individualized sleep, hygiene, bathroom, and other daily routines that the person prefers;
- Ensuring staff are consistent and familiar to the individual;
- Physical and cognitive exercises; and
- Many types of therapy (music, aroma, reminiscence, behavioral, pet, light, etc.).[56]
Fundamentally, many of these interventions are ways of making an institutional environment conform to an individual’s needs; it is the converse that can give rise to distress, discomfort, and disorientation. Older people and people with dementia should be included and consulted on non-pharmacologic alternatives and other matters that affect their lives and well-being. Including residents shows that their opinions and perspectives about their own care are respected and valued. Even when people with cognitive disabilities have difficulties expressing themselves verbally, they can often indicate some preferences otherwise.
Some medical experts believe and CMS endorses that if it is not possible to address underlying medical, physical, social, or environmental factors in some people, an antipsychotic drug “can minimize the risk of violence, reduce patient distress, improve the patient’s quality of life, and reduce caregiver burden.”[57] The evidence of the effectiveness of nonpharmacologic intervention is mixed.[58] According to the American Psychiatric Association, which issued practice guidelines on the use of antipsychotic drugs in people with dementia, the “expert consensus suggests that use of an antipsychotic medication in individuals with dementia can be appropriate.”[59]
Yet the guidelines conclude, “in clinical trials, the benefits of antipsychotic medications are at best small.”[60] Meanwhile, countering these meager potential benefits is the “consistent evidence that antipsychotics are associated with clinically significant adverse effects, including mortality.”[61] The risks vary depending on the type and stage of dementia, other conditions the person has; other drugs the person takes; the dosing and duration of the antipsychotic drug; and the particular antipsychotic drug.[62]
Similarly, CMS has warned against inappropriate use of antipsychotic drugs, given the risks that are unwarranted when the drugs do not serve a medical purpose:
It has been a common practice to use various types of psychopharmacological medications in nursing homes to try to address behavioral or psychological symptoms of dementia (BPSD) without first determining whether there is an underlying medical, physical, functional, psychosocial, emotional, psychiatric, or environmental cause of the behaviors…. When antipsychotic medications are used without an adequate rationale, or for the sole purpose of limiting or controlling behavior of an unidentified cause, there is little chance that they will be effective, and they commonly cause complications.[63]
Human Rights Watch uses the term “inappropriate” to describe use of the drug in older people with dementia that is: inconsistent with recommendations of medical experts and authorities, such as the American Psychiatric Association and FDA; inconsistent with federal regulations governing nursing homes, which overlap significantly with medical experts’ recommendations; and administered without free and informed consent except in cases of emergency. Concretely, “inappropriate use” in people with dementia often entails use that is not a last resort, use excessive in dose or duration, use without appropriate monitoring of side effects, or use not based on an informed choice about treatment options.
Massive Use of Antipsychotic Medications
It is essential that antipsychotic drugs be used cautiously in people with dementia, only where medically appropriate, and only with informed consent because of the propensity for nursing facilities to use the drugs for non-medical purposes and because of the high risk and low likelihood of benefit even when used for medical reasons. However, Human Rights Watch’s analysis of data on the prevalence of use in people without “exclusionary diagnoses” and interviews with this category of people strongly suggest that such limited use is not what occurs in practice.
Nursing facilities in the US use antipsychotic medications on a massive scale. Every week, facilities administer antipsychotic drugs to over 179,000 long-stay residents (residing in the facility for more than 100 days) who do not have an exclusionary diagnosis—of schizophrenia, Huntington’s disease, or Tourette syndrome, psychiatric and neurological diseases for which the drugs are approved—and most of whom have dementia.[64] At the end of 2016, CMS’s official measure was that 16 percent of long-stay nursing home residents were receiving an antipsychotic medication without one of these three exclusionary diagnoses.[65]
While the national average rate of use of antipsychotic medications among older people in nursing facilities without an appropriate diagnosis has declined in recent years, current prescription rates vary significantly across the country (see Map 1).
Antipsychotic medications not only have adverse medical consequences, but also have social and emotional effects on nursing facility residents and their families. To capture these consequences of forced and inappropriate antipsychotic drug administration, Human Rights Watch interviewed people living in nursing facilities who had dementia and were currently on antipsychotic medications or had been on them previously, as well as their family members. We spoke with 74 residents and 36 family members in all six states. Residents described the trauma of losing their ability to communicate, to think, and to remain awake. Family described the pain of witnessing these losses in a loved one.
Of course, dementia itself causes significant losses, affecting cognition, communication, memory, and other functions. It is impossible without a comprehensive medical evaluation, if then, to determine the direct cause of any individual changes in residents described here. However, most or all antipsychotic drugs in people with dementia are associated with sedation and fatigue.[66] (The type, dose, duration, drug-drug interaction, and other characteristics of antipsychotic drug treatment, as well as a person’s health condition aside from dementia, influence the effects the medications have.[67]) Family members described cognitive and energetic improvements once antipsychotic drugs were stopped—even if the underlying dementia persisted.
Many of the following cases illustrate the psychosocial harm associated with sedation.[68]While they are not testimonies from medical experts who could authoritatively conclude that the antipsychotic drugs caused the sedation described, these descriptions by residents and family members are representative of what antipsychotic drugs in older people with dementia often induce.[69] Moreover, in each of the following cases (except one where the individual took the drugs until she was receiving hospice care and died), the sedative effect ceased when they stopped taking antipsychotic drugs.
Ruth D., a 62-year-old woman who said she was given Seroquel (an antipsychotic medication) without her knowledge or consent in a nursing facility in Texas said: “[It] knocks you out. It’s a powerful, powerful drug. I sleep all the time. I have to ask people what the day is.”[70] The woman described being given the medication against her will, including in her food: “They crush it so you don’t know what you’re getting fed.” When asked to take Seroquel, she would tell nursing staff that she did not want to take it, and that she did not want to eat the food if she suspected the drug was in it. Ms. D continued to object as well as she could to being administered antipsychotic drugs until her discharge from the nursing facility the day after Human Rights Watch interviewed her.
Walter L., an 81-year-old man told Human Rights Watch that antipsychotic medicines “get me so I can’t think.”[71] According to his wife, Anna L., who is his healthcare proxy, he was given them without his or her knowledge or consent. Mr. L told Human Rights Watch that he never again wanted to take something that made him “change the person that I am.” Ms. L. described that when her husband was on the medications he was just “staring straight ahead,” not knowing she was even there. “I leaned him up against the wall, I came back three hours later, and he had not moved,” she said.[72] Ms. L. learned of the drug after a nurse privately alerted her. After changing facilities, the antipsychotic drug was discontinued.
Madeline C., an 87-year-old woman in a facility in Illinois, described the effect of antipsychotic medications administered in a prior nursing facility. She had been placed in a dementia unit. The woman said that when she “just about went crazy” from being in a locked unit with no activities, she “started speaking out, saying things were not right.” After that, she said, “suddenly I was very sleepy,” adding, “you feel like you’re going to die there.” She said she later learned that the facility had given her an antipsychotic drug. At the time of the interview, the woman was in a different facility that had discontinued the drug. “The fog lifted…. There’s the old Madeline again.”[73] Being at the prior facility was “a very traumatic time.”[74]
Alma G., the sister and power of attorney of Mariela O., an 84-year-old woman with dementia who died in 2017, said that her sister’s nursing facility gave her an antipsychotic drug to ease the burden of bathing her.[75] She said, “They give my sister medication to sedate her on the days of her shower: Monday, Wednesday, Friday—an antipsychotic. They give her so much she sleeps through the lunch hour and supper.”[76]
Kirsten D., the daughter and power of attorney of Joan D., a 75-year-old woman in Kansas, said that when the nursing facility began giving her mother antipsychotic and other psychotropic medications, “she would be asleep when I visited. She slept a lot. They’d say she’s adjusting to the meds. I went back weeks later. She would just sit there like this.”[77]
Joan D. said that she tried to avoid taking the antipsychotic drugs—including by hiding them in her dinner roll—because of their effect on her. “I didn’t want to take it so I didn’t. I didn’t want to feel that way.”[78] She explained further that “I try not to take it. Sometimes I have to.”
Kirsten D. described her mother on the antipsychotic medication as “no personality. Just a zombie…. The fight is gone. It’s gone. That’s what worries me the most…. I think she’s learned to keep it contained. She was vibrant, full of life…. She’s still in there.”[79] After significant effort to find another facility with an opening that would accept her mother, Ms. D. moved her mother to another nursing home that ceased the medication. Ms. D said that her mother became lively, talkative, friendly, and mobile again without the medication.
In New York, Dorothy R., the daughter and power of attorney of a woman in a nursing facility, told Human Rights Watch that a nurse informed her that the sudden decline in her mother’s health and cognition was due to her mother “getting older.” After an advocate’s lecture on antipsychotic drugs alerted her to the impact of antipsychotic drugs, Ms. R. requested a list of all the medications her mother was taking. She succeeded in having the facility discontinue the administration of an antipsychotic drug after discovering that the facility had put her on one without her or her mother’s knowledge or consent.[80]
In several cases, we documented how people with dementia seemed to improve dramatically once the antipsychotic drugs were discontinued. Laura F., the daughter of a resident in California, initially saw her mother’s decline as an irreversible, progressive result of her age: “You know, she’s 90. Yesterday, she’s alert. Now she’s not. That’s what happens.”[81] But when the nursing facility took her mother, Selina C., off Risperdal, the antipsychotic medication she had been on for over two years at that point, Ms. F. said the mother she had known returned:
Lo and behold, she can talk again. She can read again … she’s conversing … it’s not just that she can walk now … it’s her personality. She came back. She had been sleeping all the time. She was totally incoherent. She had no memory at all. She recognized no one. On the meds, she couldn’t remember if you were there while you were there…. She was drugged![82]
In this case, the antipsychotic medication had been initiated in a board and care home (similar to assisted living but smaller, with only six or fewer residents). Ms. F., her mother’s power of attorney, had consented to their use but had not been given full information about their side effects and risks. Upon Ms. C.’s admission to a nursing home, staff continued the antipsychotic drug. Once Ms. F. learned of its potential harm and insisted that the facility stop giving it to her mother, staff complied.
Human Rights Watch also visited some facilities that significantly reduced levels of antipsychotic drug use in the last year as a result of federal and state educational and training efforts, or due to governmental or corporate owners’ pressure. Interviews with nursing home administrators, directors of nursing, and other nursing staff provided another angle of insight into the extent to which antipsychotic drugs are used inappropriately. In many cases, staff of nursing homes that had reduced the use of antipsychotic drugs now felt very strongly that the drugs not be used inappropriately.
The director of nursing at one facility in Kansas who led an effort to reduce the rate of antipsychotic drug use in people with dementia reflected on the experience to Human Rights Watch: “It used to be like a death prison here. We cut our antipsychotics in half in six months. Half our residents were on antipsychotics. Only 10 percent of our residents have a mental illness.”[83] She continued:
Some doctors are misinformed. When we said we wanted to reduce the antipsychotics, we had to fight with the doctor. He said: ‘You understand if I do this they’re all going to go crazy?’
But they don’t have behaviors because they need an antipsychotic. You actually see them decline when they’re on an antipsychotic. It’s just an adjustment when they’re first admitted.
There was a woman who would stand at the nurse’s station sobbing. We should have done a root cause analysis. But instead we shipped her off to psych. She was gone within a year: stiff muscles, couldn’t walk or talk. I think it’s sadder than watching someone with dementia decline.
You can reduce antipsychotics…. Residents have behaviors because their needs are not met. Not because of a lack of staff. We reduced the rate drastically and haven’t had to change staffing levels one bit. We did increase staff for activities, but not CNAs [certified nurse aides].
Taking off antipsychotics affects people differently: some are more verbal, more disruptive, louder, but not violent. Some sleep more, some sleep less. We had to educate the staff: don’t put them back on immediately. All antipsychotic prescriptions go through me. I do not allow PRN [prescription to take as needed] antipsychotics. Giving someone a Haldol one time has never been effective. It has to build up in the system.[84]
At another facility in Kansas, a nurse told Human Rights Watch about their experience reducing use, echoing many of the same themes:
We were at 55 percent antipsychotic drug rate before. Now we’re down to only people with a diagnosis [for which the FDA has approved the medications] on the drugs. They have a better quality of life because they’re not sedated. We’re not controlling their emotions or their dementia.
At first everyone was like, ‘This is going to be awful. What do they want us to do?’ But we started with a resident with fewer behaviors and just did one or two a week. It was amazing. It’s helpful: it actually minimizes behaviors.
Before, when we slapped them with antipsychotics, they had to be in a wheelchair because they were so drugged up. But now that we’re meeting their needs, it’s easier on staff…. Their ADLs [activities of daily living] are better, their functioning.
If a resident comes in on an antipsychotic, we go over the info. We say, ‘We don’t usually use those here.’ The family usually agrees. If we start the reduction and it doesn’t work, we tell a geriatric psychiatrist to see them once a week. We have not had to change our staffing numbers. Without the antipsychotics, the residents take less time.[85]
In Illinois, the director of nursing at a facility explained a similar course of action:
This is our biggest, biggest issue: taking people off. You have to make an attempt to reduce. If someone is taking two antipsychotics, you try to lower the dose and you try taking them off one. We attempt reductions quarterly. We have not had problems with behaviors after slow reductions…. The pharmacist sends a report monthly, giving recommendations [to reduce] every month….
We used to have a big antipsychotics problem. In 2011 more than half of the residents took them. Now everyone on an antipsychotic has a diagnosis. Usually they’re a totally different person, they’re back to life.[86]
An administrator in California described procedures his nursing facility has put in place to reduce reliance on antipsychotic medicines:
Our psychotropic committee meets monthly. We review all the patients on psychotropics. In 2010, more than 30 percent of the residents were on antipsychotics. Now it is just over 10 percent…. If someone is admitted with an antipsychotic, we monitor them for 72 hours. We notify the doctor. We observe the behavior. [Our consultant psychiatrist] comes in to assess if it’s necessary. We gather the baseline to have a point of comparison. We look at the diagnosis. If we get someone from geri-psych, they’re often agitated in the unit. Their behavior is not consistent. We put psychotropic medication on hold. We don’t restart it. We give them a chance to adjust.[87]
| Inside Nursing Facilities with High Rates of Off-Label Antipsychotic Drug Use
The conditions in about 20 of the 109 facilities visited, across all six states, were disturbingly grim. It was not uncommon for facilities to have stenches of urine, in particular on locked dementia units. Many facilities visited on weekends appeared to be severely understaffed. Many facilities were located in old buildings, sometimes former hospitals. The bare, cinderblock rooms—with uniform, old furniture and no privacy except a curtain with a runner on the ceiling—feel like “wards,” though use of the word is discouraged. People were often heard screaming or calling for help. Call light alarms—buttons residents can press that produces sound and light up at a nursing station to alert staff—would often make noise unceasingly. Human Rights Watch researchers encountered residents who desperately needed an aide to help them use the bathroom. In one case, we observed a nurse aide walk past a resident lying on the floor exposed, proceeding to carry a food tray. In several cases, residents had bruised faces or eyes that staff seemed unable to explain.
Researchers observed individuals apparently trapped in “geri-chairs,” a geriatric recliner chair positioned in such a way that they could not get out. Positioning someone in this way constitutes a physical restraint.[88] Many people’s heads rested on tables or on their chests. Residents slept on couches in the lobby. It was unusual to visit a facility in which people were not sitting in wheelchairs arranged around a nursing station. Human Rights Watch staff observed very few activities aside from meals and television.
Many facilities evinced a startling lack of privacy. Nursing staff enter residents’ rooms unannounced. We often saw staff who failed to close residents’ doors before engaging in tasks that exposed them, such as continence care and some types of therapy. Human Rights Watch observed residents being pushed in wheelchairs to shower rooms with only a sheet draped across their front. We observed residents moving about the facility with catheter bags exposed. |
BACK TO TOP
III. Inappropriate and Non-Consensual Use of Antipsychotic Medications
The inappropriate use of antipsychotic drugs on people with dementia in nursing facilities raises two principal human rights concerns. First, antipsychotic drugs are often administered without a medical purpose—as a last resort to treat psychosis in dementia, although they have not been found to be effective to this end—and for the convenience of facility staff. Such medically unnecessary use of medication may amount to torture or ill-treatment under international law. It may also amount to a prohibited “unnecessary drug” or a chemical restraint—a form of abuse—under US law. Second, these medications are frequently administered without free and informed consent. This practice constitutes forced medication under international law.
Chemical Restraints and Unnecessary Drugs: Use of Antipsychotic Medications for Reasons Other than Medical Need
Antipsychotic drugs are frequently administered to older people with dementia without clinical indication (a valid medical reason). This practice may in some cases rise to the level of torture or cruel, inhuman and degrading treatment. As noted by the UN special rapporteur on torture and other cruel, inhuman or degrading treatment or punishment in a 2013 report: “medical treatments of an intrusive and irreversible nature, when lacking a therapeutic purpose, may constitute torture or ill-treatment when enforced or administered without the free and informed consent of the person concerned.”[89] In June 2017, the UN special rapporteur on the right to health noted that informed consent is “a core element of the right to health, both as a freedom and an integral part of its enjoyment.”[90]
US regulations establish that antipsychotic drugs cannot be administered to nursing facility residents without a medical need based on a comprehensive assessment.[91] However, in some facilities, medical need is often not the primary reason antipsychotic drugs are prescribed and comprehensive assessments are not routinely conducted to determine whether a medical basis exists. CMS recognized facilities’ improper use of the drugs:
It has been a common practice to use various types of psycho-pharmacological medications in nursing homes to try to address behavioral or psychological symptoms of dementia (BPSD) without first determining whether there is an underlying medical, physical, functional, psychosocial, emotional, psychiatric, or environmental cause of the behaviors.[92]
Interviews with residents, family members, and facility staff provide numerous examples that residents are administered antipsychotic drugs without meaningful assessment of their medical necessity—an important consideration, though not one that, alone, justifies administering the medication.
A Culture of Antipsychotic Medication Use
Government reports and academic literature identify a “culture” of antipsychotic drug use as one of the potential explanations for their widespread use. In this context, the “culture” of a nursing facility, meaning the “shared values, beliefs and assumptions” of staff, “may exhibit itself as a facility-level preference for certain therapeutic modalities.”[93] When the prescriber and individual receiving treatment interact infrequently, which is often the case in nursing homes, the general treatment approaches may take on heightened significance: without routine personal evaluations by a physician prior to medication decisions, these decisions may follow even more heavily from the existing “beliefs and assumptions” about treatment, and may be less specific to the individual and circumstances at hand.[94] A 2015 study by the US Government Accountability Office (GAO) found that so-called setting-specific factors—such as staff leadership, training and education levels, and quantity of staff—were the principal determinants of the prevalence of antipsychotic drug use rather than patient-specific factors, such as medical conditions or behaviors.[95] Academic studies have found that facility characteristics—not just a resident’s behavioral or neuro-psychiatric symptoms—are a strong predictor of the prevalence of psychotropic medication use.[96] One study found that “new nursing home residents admitted to facilities with high antipsychotic drug prescribing rates were 1.4 times more likely to receive antipsychotics, even after controlling for patient-specific factors.”[97]
In facilities with such a culture of the widespread use of these medicines, the off-label drug use is generally accepted as typical and unproblematic—even the best course of action for the resident. The GAO study found that in such facilities, nursing staff are more likely to believe the medications are truly helpful to residents, and are more likely to have lower levels of education and training around dementia and appropriate use of antipsychotic medicines. Studies have shown that low education among staff about antipsychotic use among people with dementia results in higher rates of use.[98] The GAO report also found that insufficient staff to engage residents in activities and to provide oversight of them may “make the nursing home residents susceptible to higher antipsychotic drug use.”[99]
In a letter to Human Rights Watch, the American Health Care Association (AHCA), the for-profit nursing home trade association, wrote:
[The] biggest challenge we have found is the mindset that clinicians, nurses and family all have that ‘behaviors’ in dementia are abnormal, resulting from dementia and that medications are an effective treatment. Difficulty in changing this belief is the greatest challenge.[100]
To this end, the AHCA has produced a fact sheet on antipsychotic drugs and people with dementia to inform families about the dangers and ineffectiveness of their use.[101]
Human Rights Watch obtained testimony from staff suggesting a culture in some facilities of excessive antipsychotic drug use in residents. In Texas, a facility’s admissions director seemed to believe that residents should be given the medication: “It’s a red alert if they don’t take them. We try to get them to.”[102] A nurse at a facility elsewhere in Texas, said: “If they’re agitated or having a moment and they don’t have a prescription, we call the doctor or psychiatrist…. If we still can’t handle them, we send them to behavioral [a psychiatric hospital].”[103]
Lena D., the daughter and power of attorney of Lucinda D., an 88-year-old woman in a California nursing facility, said she felt that the facility only attempted to silence with antipsychotic medication the symptoms that disturbed staff. To Ms. D, it was obvious that her mother had physiological conditions, such as an infection causing smell and fever, requiring medical attention instead of antipsychotic drugs to dull the expression of distress. “Every little thing, they want to put you on psych meds,” she said.[104] Ms. D. said that her mother was screaming from pain. “She would be sitting there, slumped over, mucus everywhere. I would go over and say, ‘She’s sick.’ UTI [urinary tract infection], pneumonia, pulmonary embolism—I’d scream too,” Ms. D. said, listing a number of the infections and harms she says that her mother has endured.[105]
In many instances, people living in nursing facility and their relatives—like most people—are inclined to defer to the recommendations of the healthcare provider unless they have a reason not to do so. As one long-time expert in Kansas put it: “The family rarely objects. They think, ‘They’re the doctor. They’re not going to hurt my mom.’”[106] A nurse in Texas explained: “If the medication is on the psychoactive list, we need consent.[107] We call the guardian, get verbal consent. Or not, if it’s declined. Then we’d call the doctor and start over. But we’ve never had to deal with a decline. Families want the best, and they trust the physician to do that.”[108]
This trust can backfire in some nursing facilities. Contrary to other contexts, doctors and nurses associated with nursing facilities may favor the easier step of a prescribed medication than more time-consuming interventions. In some cases, medical and nursing staff may truly believe in the utility of the medications in situations where their use is inappropriate. Lastly, the tendency to trust doctors may be problematic in the context of nursing facilities where physicians interact with their patients very rarely even when they are prescribing antipsychotic drugs.
Antipsychotic Medication Use for the Convenience of Staff
In line with international human rights law, US law and regulation prohibit the use of antipsychotic medicines as a chemical restraint on residents—i.e., when drugs are “used for purposes of discipline or convenience, and not required to treat medical symptoms.”[109]Interpretive guidelines of federal regulations define “convenience” as “any action taken by the facility to control a resident’s behavior or manage a resident’s behavior with a lesser amount of effort by the facility and not in the resident’s best interest.”[110]
While most staff we interviewed were adamant that they do not use antipsychotic or other medications for their own convenience, a few admitted to exactly that. A social worker at a facility in Texas, for example, said: “You have got to get through incontinent care and the shower. We give meds before their showers…. We give them something they’re taking already. We just want to make sure it’s in their system when we’re showering them.”[111]
While nursing staff may face real challenges providing such direct care to some people, turning to antipsychotic medications is not appropriate. As the CMS State Operations Manual explains, to comply with federal regulations, facilities must find ways to accommodate individuals’ preferences:
If the resident refuses a bath because he or she prefers a shower or a different bathing method such as in-bed bathing, prefers it at a different time of day or on a different day, does not feel well that day, is uneasy about the aide assigned to help or is worried about falling, the staff member should make the necessary adjustments realizing the resident is not refusing to be clean but refusing the bath under the circumstance provided.[112]
Generally, as the revised CMS State Operations Manual states:
In some cases, resident with dementia may resist the manner in which care is being provided, or attempted, which can be misinterpreted as declination of care. In some cases, the resident with dementia does not understand what is happening, or may be fearful of unfamiliar staff, or may be anxious or frustrated due to inability to communicate.[113]
It is a responsibility of facility staff to “attempt to identify the underlying cause of the ‘refusal/declination’ of care.”[114]
Many outside observers, such as long-term care ombudsmen, academics, and state inspectors, told Human Rights Watch that antipsychotic medications were being used for the convenience of staff. A social worker at a behavioral hospital in Texas explained their perspective on nursing facilities’ use of antipsychotic medications for staff convenience, as chemical restraints:
People come in here [a hospital] for behaviors, but then we don’t see the behaviors when they’re here. Sometimes we change their meds. But they don’t usually exhibit horrible behaviors. Maybe they just need attention. But the nursing homes don’t want behaviors. They want docile. They want people with no cognitive deficits who can take care of themselves. I’ve worked in nursing homes. They’d say, ‘Send them to [the psychiatric hospital] to get medicated and let them come back.’[115]
A state inspector with a long career in long-term care said: “I see way too many people overmedicated. The doctor signs off and the nurse fills the prescription. They see it as a cost-effective way to control behaviors.”[116] Seventeen of 18 ombudsmen we interviewed echoed this view, including at least one from every state visited.[117]
Madeline C., an 87-year-old woman in Illinois, reflected on her time at a prior facility, which gave her antipsychotic medications against her will, leaving her in a stupor. She said: “When I was in that other place [the prior nursing facility], they just wanted you to do things just the way they wanted.”[118] An expert and advocate in Illinois explained: “Antipsychotics are often about the nursing staff, not the residents.” In requesting the medication from a doctor, nursing staff often say: “‘I need a restraint.’ It’s not just a figure of speech.”[119] In other words, it’s the staff who “need” the resident to be taking it.
Failure to Initiate, Monitor, and Discontinue Antipsychotic Medications
US law and regulations require nursing facilities and healthcare providers to have an adequate medical basis for initiating antipsychotic medications and for continuing use. Regulations prohibit the use of any “unnecessary drugs,” defined as:
- In excessive dose, which can be determined based on a manufacturer’s label;
- For excessive duration, meaning beyond the manufacturer’s or clinical studies’ recommended period of use; and/or without evidence of additional therapeutic benefit;
- Without adequate monitoring;
- Without adequate indications for use: “the identified, documented clinical rationale for administering a medication that is based upon an assessment of the resident’s condition and therapeutic goals”;
- In the presence of adverse consequences indicating the medication should be reduced or discontinued. Adverse consequences include “unpleasant” symptoms or events, including “impairment or decline in an individual’s mental or physical condition or functional or psychosocial status.”[120]
Federal regulations particular to psychotropic drugs mandate that any prescription for someone not already taking such medication must be “necessary to treat a specific condition as diagnosed and documented in the clinical record.”[121] Anyone given psychotropic medications must “receive gradual dose reductions, and behavioral interventions, unless clinically contraindicated, in an effort to discontinue these drugs.”[122]Gradual dose reduction must be attempted annually, except twice in the first year of use.[123]
These regulations represent an attempt to limit and regulate the use of antipsychotic drugs in ways that would help protect the human rights of nursing home residents if facilities adhered to the regulations. One of the most recent government studies on resident assessments and care planning—the foundation for determining what antipsychotic drug use could be appropriate—found that few facilities comply with relevant regulations. The 2012 Office of Inspector General of the US Department of Health and Human Services report found that 99 percent of the records reviewed of older nursing facility residents (aged 65 and older) receiving antipsychotic drugs in 2007 failed to meet at least one federal requirement for resident assessments and care planning.[124] Human Rights Watch’s research and a review of governmental surveyors’ narrative deficiency reports found that these procedures and limitations required for appropriate psychotropic drug use are often ignored.
Many of our interviews tend to bolster the contention that antipsychotic medications are often prescribed to nursing home residents for no valid medical reason. Some nursing staff described to Human Rights Watch the primary “behaviors” for which antipsychotic medications are frequently used. A nurse at a facility in Kansas said that “calling names, screaming, scaring people” justified antipsychotic medication.[125]
In Texas, a social worker said that the most common “behaviors” leading to antipsychotic medication use were: “‘Son of a bitch.’ ‘Help me, help me, help me.’ It’s not having a filter.”[126] A long-term care pharmacist in Kansas said he routinely sees medication requests without an appropriate diagnosis. “This is a sore spot,” he said. “I write letters to the nursing homes and prescribers because there’s no supporting diagnosis for an antipsychotic at all. It just says ‘Seroquel for dementia,’ or ‘Seroquel for anxiety,’ or ‘Seroquel for behavior dysfunction.’”[127]
A 2005 study found that about one in three nursing facility residents covered by Medicare took medication in excessive doses and lacking appropriate indications.[128] The US Department of Health and Human Services Office of Inspector General report from 2011 found that 51 percent of Medicare atypical antipsychotic drug claims—the second generation of antipsychotic drugs, commonly used for their perceived lesser side effects—for older people in nursing facilities “were either not used for medically accepted indications as supported by the [medical] compendia or not documented as having been administered to the elderly nursing home residents.”[129] The Office of Inspector General review of 1.4 million antipsychotic drug claims for older residents found that 22 percent “were not administered in accordance with CMS standards regarding unnecessary drug use in nursing homes.”[130]
A review of surveyors’ narrative deficiency reports provides examples of facilities’ failure to comply with requirements to monitor, taper, and discontinue antipsychotic drugs. For example, in New York, in 2016, government surveyors issued a deficiency citation for unnecessary drugs because a nursing facility prescribed a “standing dose” of an antipsychotic drug for “wandering, noncompliance, and aggressive behaviors” to a man who had no history of taking antipsychotic drugs. The dose was increased from twice a day to three times a day within one week and surveyors concluded it contributed to the man’s death within 10 days.[131]
In Illinois, in 2015, an inspector issued a deficiency citation for unnecessary drugs for a facility’s “failing to have indications for use, assessing, identifying/monitoring targeted behaviors, clinical rationale for the medication dosage use above the recommended level, and completing a Gradual Dose Reduction (GDR)” for an antipsychotic drug.[132] The excessive dose of an antipsychotic without an appropriate diagnosis in a person with dementia led to the person’s “being continuously somnolent” and falling repeatedly, according to the government surveyor. The individual’s records show that, in less than five months, the individual fell eight times, the last time leading to an irreparable condition and the person’s admission to hospice.
In Texas, in 2015, government surveyors issued a deficiency citation for unnecessary drugs based on a facility’s giving a woman “excessive doses” of an antipsychotic drug, not adequately monitoring her, and giving the drug without an appropriate diagnosis.[133] As a result of the facility’s failure to comply with unnecessary drug regulatory requirements, the woman was hospitalized for septic shock. Nursing staff described the woman’s decline to government regulators: she was “alert, oriented…, could feed herself, and could carry on conversations” when she was admitted. After the excessive medication, the woman could not bear her own weight or “stay awake to eat or drink.” Staff corroborated that no nonpharmacologic interventions were attempted and no behavioral monitoring occurred.
Interviews and a review of national nursing home data also suggest that some facilities are circumventing pressure to reduce inappropriate use of antipsychotic drugs by inappropriately seeking a diagnosis from a physician of a medical condition, such as schizophrenia, for which these medicines are approved in order to not raise red flags when prescribing someone antipsychotic medication inappropriately. The onset of bipolar disorder and schizophrenia rarely occurs in people over the age of 30.[134] Thus, experts are concerned that the uptick in schizophrenia diagnoses in older people in nursing facilities—from 6.53 percent in the fourth quarter of 2011 to 8.49 percent in the second quarter of 2017, a 30 percent increase in less than six years—is indicative of facilities adding a diagnosis to justify the use of these medicines.[135]
In a joint statement, numerous organizations, including the American Association for Geriatric Psychiatry, American Association of Nurse Practitioners, American Geriatrics Society, American Health Care Association, American Medical Directors Association, Society for Post-Acute and Long-Term Care Medicine, American Psychiatric Association, and LeadingAge, responded to this uptick.
While there is a national need for better and more approved treatments for behavioral and psychiatric symptoms in dementia, clinicians need to be mindful of and avoid labeling patients with other diagnoses to justify the use of medications or other treatments.[136]
In Kansas, the daughter and power of attorney of a 75-year-old woman learned that the facility had begun “giving her meds for bipolar”—a diagnosis she first received at age 74. In California, a nurse stated:
If they’re coming from an acute hospital (a hospital providing care to individuals experiencing or recovering from acute episodes of illness, injury, surgery, or trauma), they have a diagnosis. We can’t admit them otherwise. Sometimes we go around with the hospital to get us a psych diagnosis.[137]
In Texas, a social worker at a nursing facility said: “Since you’re taking that medicine, then you get a diagnosis. That’s how you get a diagnosis. If we’re treating the symptoms, then you have the disease.”[138]
| Other Discriminatory Ways Nursing Facilities Treat “Difficult” Residents
Administering antipsychotic drugs inappropriately is not the only way nursing facilities mistreat people they consider to be “difficult.” Human Rights Watch’s research found numerous instances where facilities sought to avoid admitting or to discharge such people pretextually in apparent violation of federal regulations which require facilities to “provide equal access to quality care regardless of diagnosis, severity of condition, or payment source.”[139]
Expressing a sentiment we heard in many interviews with nursing facility staff, the director of nursing at a facility in Texas said: “Nursing homes do not want patients with behaviors.”[140] In the words of a long-term care ombudsman in Kansas, “a ‘behavior’ is not being quiet.”[141] In Texas, another long-term care ombudsman explained:
A resident is ‘disruptive’ if she’s outspoken: if she’s not happy with what they’re doing. Even if the family is outspoken, that’s a problem…. I get complaints all the time from facilities: residents refusing to get up, not wanting to go to an appointment. They’ll say she’s not cooperating, refusing care. Basically, ‘disruptive’ means a person knows her rights.[142]Administrators, nurses, and social workers said that they review a potential resident’s “behaviors” prior to admitting them. A director of nursing in Kansas said: “If they’re cognitively impaired, controlling, manipulative, we try to not take them in the first place.”[143] A director of social services at another facility in the state said: “If we can identify someone’s behaviors before admission, we won’t touch them. The best time to ‘discharge’ though is before we even admit them.”[144] An administrator in California summed it up: “Once you admit them, they’re your liability.”[145]
Facilities sometimes also try to transfer or evict people contrary to their rights. A retired long-term care ombudsman in Kansas said that facilities weigh costs and benefits of wrongful discharges and the possibility of being penalized for them. “Some nursing homes will say, ‘I’ll take the deficiency just to get rid of them.’ They’ll discharge people to homeless shelters.”[146]Since 2010, involuntary discharges have been the top category of complaint that long-term care ombudsmen receive.[147]
The great-grandson of a 92-year-old woman in Texas described how his great-grandmother was “dumped three times” from nursing homes, with two psychiatric hospitals in between, before going to two additional nursing homes, the last of which threatened to send her to another hospital.
When I picked her up from the last facility, she had the biggest knot on her head…. She has fallen so many times. She has never been hurt badly. But she always has knots. They never sent her to a hospital for that. Every right she has, has been violated. To me, it’s wrong. She is 92 years old.[148]His great-grandmother was living with him, instead of a nursing home, at the time of the interview. |
Failure to Obtain Free and Informed Consent
I don’t take Seroquel. I take Clonidine for cholesterol, something for my heart and blood. But I don’t take Seroquel. It is nowhere in my record.
—Ruth D., a 62-year-old woman in a nursing facility in Texas, December 2016[149]I don’t think antipsychotic drugs are presented well to the family in informed consent conversations. Because if it were, they’d all reject it. And when they [staff] don’t inform them beforehand, then the family is not having a real choice.
—A long-term care pharmacist in Kansas, January 2017[150]
International human rights standards require that any medical intervention be provided only with free and informed consent.[151] At its foundation, this right arises from an individual’s right to decide what is done with his or her own body.[152] Free and informed consent—contrary to mere consent: written or oral permission, however it is obtained and whatever its basis—requires a full understanding of the purpose, risks, benefits, and alternatives to the medical intervention, and the absence of pressure or coercion in making the decision.[153]
US federal regulations, including revised regulations that intended to go into effect on November 28, 2017, state that nursing home residents have the right to be fully informed in advance of their treatment and have the right to refuse treatment.[154] Combining the right to be informed with the right to refuse treatment, individuals should have protection that is substantially similar and potentially equal to informed consent if enforced effectively.
Obtaining free and informed consent for medical interventions can pose significant challenges for doctors and nurses whose patients are in nursing homes. A large percentage of people who live in these institutions experience dementia or other conditions that affect their cognitive abilities. Many people in nursing facilities do not make their own decisions about their treatment.
In some cases, people are formally stripped of legal capacity, meaning the authority under law to exercise one’s rights and to make decisions for oneself, and another person acts as a surrogate decision-maker.[155] (Under US regulations, the rights to be fully informed in advance about treatment and to refuse treatment apply only to residents that have not been formally “adjudged incompetent” and who do not have a surrogate authorized to stand in on these subjects.[156]) More commonly, doctors either informally determine that people are not competent to make decisions about their care, or doctors and staff discuss care issue with relatives or health proxies by default, regardless of the resident’s cognitive abilities and the scope and activation of the proxy.
Proxies are legal devices to protect “prospective autonomy.”[157] Instead of being formally adjudicated to lack capacity, many people voluntarily designate in advance, under state law, another person—termed a proxy, agent, healthcare representative, advanced directive, attorney-in-fact, legal appointee, or durable power of attorney for health care—to support them in decision-making or to act in their stead and carry out their wishes upon a certain stage of cognitive disability.[158] However, these legal representatives are limited in scope and time. The proxy authority is activated only during the period of lost capacity and only on the specified subjects or decisions: “Any decision-making power that is not legally granted to a representative under state law is retained by the resident.”[159]
The formal loss of legal capacity and excessive or premature use of proxies can completely exclude people from decisions that have major implications for their health. In some cases, this deprivation happens even when the person concerned does not have significant cognitive disabilities. For example, a former Kansas long-term care ombudsman said: “The nursing home sometimes goes straight to the POA [power of attorney] when the resident still has capacity. I often had to remind the nursing home that the POA is not all-encompassing.”[160] As the revised federal regulations state: “Determinations of capacity to consent depend on the context of the issue and one determination does not necessarily apply to all decisions made by the resident.”[161]
| Legal Capacity, Informed Consent, and the Convention on the Rights of Persons with Disabilities
The Convention on the Rights of Persons with Disabilities (CRPD), which the US has signed but not ratified, seeks the abolition of substituted decision-making in favor of supported decision-making and rejects the concept that any person can be deprived of legal capacity because of a disability.[162] Unlike substituted decision-making—in which a second person supplants the individual whose decision is concerned—in supported decision-making, a second person provides whatever assistance is necessary to enable the individual to continue to make all his or her own decisions, except in situations of emergency. Thus, under this new CRPD paradigm, the role of healthcare providers and family members should in all cases be to assist people in making their own decisions, rather than to make decisions on their behalf.
While the US has not ratified the CRPD, it can and should take steps to expand and better protect the rights of people with disabilities, and the Convention is an important source of authoritative guidance.[163] Though current federal nursing home regulations fall short of what the CRPD envisions, even under current federal nursing home regulations, individuals with cognitive disabilities generally can and should be centrally involved in care planning and medical decision-making. As this report shows, far too many nursing homes fall woefully short in this regard.
In many cases, facilities can also do far more to avoid any question of a resort to substitute decision-making by anticipating the progression of a condition like dementia and engaging in advanced care planning. Individuals who may struggle in the future to participate meaningfully in decisions about their own care can be helped to develop plans laying out their wishes in the event of different possible future scenarios. Informed consent should occur within the person-centered, care planning process that begins, per regulations, upon a person’s admission to a facility.[164] |
A small percentage of people in nursing facilities make up the most complex cases: they have a cognitive disability that compromises their ability to provide informed consent and do not have any family members or other support persons, designated or otherwise, to assist them in making medical and other decisions.[165]
Most of the cases documented in this report do not fall into the category of highly complex ones. The nursing facility residents whose testimonies on the use of antipsychotic drugs appear in this report did not have significant cognitive disabilities. In our conversations with them, they seemed to understand their situation and to express their preferences regarding—and objections to—antipsychotic drugs. In other cases, the residents had designated a relative as their health proxy.
Yet we found that even in these cases where it clearly would have been possible for nursing facility staff and attending physicians to seek informed consent, doctors and facility staff failed to seek it from the individual or their proxy. In some cases where a health proxy was heavily involved in the individual’s care, the facility or practitioner sought consent but never provided sufficient information for consent to be informed.
In Texas, for example, Human Rights Watch interviewed a woman, Ruth D., 62, in a nursing facility who was given antipsychotic drugs without her or anyone’s consent, despite Ms. D.’s ability to give or withhold consent and objection to the medication.[166] Ms. D. was transferred to a nursing facility for rehabilitation after a minor stroke. After a month, the facility had not discussed care plans with her. Instead, she said, staff administered an antipsychotic medication, without informing her or seeking her informed consent.
Initially, Ms. D. said, she did not realize she was taking new medications. Once she realized, she refused to take them. She told Human Rights Watch: “They crush it so you don’t know what you’re getting fed. Put it in baby food. You know, [they put it in the] apple sauce.” As a result, Ms. D. said, “I don’t want to eat the food.”[167]
Ms. D. reported that the antipsychotic drug had had a major impact on her state of mind:
I do not mess with no Seroquel [an antipsychotic drug]. I don’t know what the drug does. But I know it’s dangerous. I was seeing monkeys on the wall… It knocks you out. It’s a powerful, powerful drug. I sleep all the time. I have to ask people what the day is… That Seroquel: that’s gonna kill me.[168]
Over the course of the interview with Human Rights Watch, nursing staff twice knocked, entered, and attempted to administer an antipsychotic drug in gel form to Ms. D. “Can I give you your medicine?” the aide said, “It’s your Seroquel.” Ms. D. replied, “I don’t take Seroquel. I take Clonidine for cholesterol, something for my heart and blood. But I don’t take Seroquel. It is nowhere in my record.”
With Ms. D.’s permission, the long-term care ombudsman, a registered nurse, and Human Rights Watch staff examined her medical chart at the nurse’s station. It did not contain any documentation that Ms. D had ever consented to taking Seroquel.
Throughout our interview, Ms. D. repeatedly stated her desire to leave the facility as she did not trust the staff and wanted to go home. “I will pay for the cab,” she kept saying.[169] The long-term care ombudsman helped facilitate her release from the facility the next morning.
In Illinois, Madeline C., 87, told Human Rights Watch that her nursing facility gave her antipsychotic medication without her knowledge or consent, or that of any family member or power of attorney. She said she never signed providing her informed consent. “I just did not know I was taking the medications. But I felt different.”[170] The woman’s family could not persuade the facility to cease the medications; instead the family eventually moved her elsewhere.
Informed consent practice varies by state and facility. Consent does not have to be obtained in writing or signed by the person providing it as opposed to nursing staff, but many facilities have informed consent sheets for residents or proxies to sign.[171]
In Texas, Dayvon G., the great-grandson and power of attorney of Nora G., said his great-grandmother’s facility had informed him they were putting her on two antipsychotic medicines. He had not objected. But the facility had failed to give him any information on the potential risks of the medications. Speaking with Human Rights Watch, he asked: “What is a black box warning? No one has mentioned it.”[172]
Rosanne J., the wife and power of attorney of Marc J., a 79-year-old man in a Texas nursing facility, said that, although she knew the medicines had a sedative effect, she was “not real familiar with anything else, if they do anything to the mind.”[173] In conversations with Human Rights Watch, she evinced an understanding that antipsychotic medication simply calmed her husband to the point of his appearing to be asleep.
Laura F., the daughter and power of attorney of Selina C., a 92-year-old woman in a California nursing facility, described having consented to antipsychotic drugs for her mother without understanding the risks: “I had no idea, not at all, that the drugs were dangerous. I had no idea. It’s on me because I didn’t know when I had agreed [to their prescription]. I’m guessing most people have no idea.”[174] When her mother was later transferred to another facility, staff there continued administering the drugs without seeking informed consent from Ms. F.
In Kansas, a long-term care ombudsman gave an example of what she said was a typical situation in a care plan meeting where facility staff wanted to put a resident on Haldol:
It’s not explained to the family. I wanted them [the facility staff] to explain the side effects. They weren’t going to tell the family that. The nursing home just said, “the resident could get aggressive, could get hurt” [if they were not put on Haldol]. So, the family agreed to put them on it.[175]
Our research suggests that in other cases, facilities that purport to seek informed consent put pressure on individuals to give consent. It is not known how common it is for facilities or doctors to use pressure to obtain consent. It is a serious abuse of the right to informed consent and of several federal regulatory requirements for those affected by the practice.
For example, Ruth D. told Human Rights Watch researchers that she feared retaliation after refusing to take the antipsychotic medication and speaking to long-term care ombudsmen about her objection to the facility’s coerced treatment. She said to the ombudsman and Human Rights Watch staff: “Once you leave I’ll be in trouble. I’m sweating.”[176]
In Illinois, a long-time advocate said: “Informed consent is telling people risks and benefits and giving them a choice. In practice, the conversation is, ‘take it or we will discharge.’”[177]For many residents, the threat of being evicted—involuntarily discharged—is real, even if federal regulations prohibit it in many circumstances.
Lena D., the daughter and designated health proxy of a resident in California explained: “If I object to the Risperdal, Seroquel, Haldol, they say, ‘okay, we are moving her.’”[178] Although the facility did not follow through on that threat, it caused Ms. D significant anxiety and made it more difficult for her to refuse the medications.
In some cases, facilities appear to play on family members’ guilt to convince them to approve the medications’ use. Christina F., the daughter of a former resident in Kansas, recounted:
The nursing home called a meeting once and said he needs meds. They didn’t present alternatives. We said, “no.” My father said he trusted my judgment. The physician’s assistant told me: “You know you’re hurting him. You’re making it worse for him.”[179]
The legitimate challenges in seeking informed consent from some nursing home residents do not excuse facilities’ failure to have an adequate standard practice of seeking informed consent. Staff from 15 nursing facilities in Texas, Kansas, California, and Florida, including administrators, directors of nursing, nurses, social workers, and social services directors, said their facilities do not seek consent generally; have no protocol for obtaining informed consent; or do not have regular discussions about these medications with residents or their relatives.[180]
Accounts of some of the residents Human Rights Watch interviewed also demonstrated a severely inadequate understanding of the meaning of informed consent among staff at nursing facilities. Ombudsmen and nursing staff explained that many facilities do no more than notify the family after the fact, with no communication with the individual concerned. One ombudsman said: “They routinely do not tell either the resident or the family [about antipsychotic medication initiation]. Or they’ll have a meeting [after the fact] and say, ‘Well, we tried to call you.’”[181] One facility’s director of nursing, the most senior medical professional in the building at most times and responsible for the administration of medications and interaction with prescribing physicians, admitted to Human Rights Watch:
We are supposed to be doing informed consent. It’s on the agenda. But really antipsychotics are a go-to thing. “Give ‘em some Risperdal and Seroquel.” We tell the family as we’re processing the order. The family is notified.[182]
In Kansas, a director of nursing, admitted: “We don’t tell someone with dementia what drug we’re giving them. That would be very good practice to do that, but in practice it’s only if they ask [that we would tell them].”[183]
A former nursing facility administrator in Kansas said:
The facility usually gets informed consent like this. They call you up. They say, “X, Y, and Z is happening with your mom. This is going to help her.” Black box warning? “It’s best just not to read that.” The risks? They gloss over them. They say, “That only happens once in a while, and we’ll look for problems.” We sell it. And, by the way, we already started them on it.[184]
A Texas state regulator told Human Rights Watch: “There is very rarely informed consent. Nurse calls [the relatives], says resident is doing this [behavior], is highly agitated. The medication is explained as ‘he really needs it.’ They [the relatives] don’t understand.”[185] A social worker at a facility in Kansas said: “There is no informed consent for antipsychotic drugs specifically. The only consent is to see a psychiatrist and to be treated. They can sign that consent at admission.”[186] While social workers are not part of the medical or nursing staff, they are liaisons between the facility staff and residents’ families and thus would be familiar with these kinds of procedures.[187]
In response to an inquiry into the facility’s informed consent procedure, one nurse at a facility in Texas told Human Rights Watch: “For informed consent, we just call to let them [the family] know. It’s verbal consent. They’ll sign it when they next come in.”[188] At another facility in the state, the social services director explained:
The doctor writes the order. The nurse calls the responsible party and says, “The doctor made a medication change. This is what the new medication is.” The [durable power of attorney] or guardian says yes or no. That’s informed consent.[189]
While the social services director would not be directly involved in this process, she appeared to explain it based on her personal knowledge of how it is done. In yet another facility, a director of nursing said, inexplicably: “Seroquel is not necessarily an antipsychotic drug. It could be an anti-convulsant. You don’t have to have consent if you’re not using it for psychotropics.”[190]
One administrator in Kansas told Human Rights Watch: “I don’t know the answer, whether we have an informed consent procedure.”[191] While facility administrators do not have to be medical professionals, they are responsible for the facility’s compliance with federal regulations, which include residents’ right to be fully informed in advance about their treatment options. They are also responsible for facilities’ compliance with state law.[192]
A director of nursing at another facility in Kansas gave her best guess on what informed consent might entail. “How do you do informed consent? I have no idea on that. Maybe call the physician, get it prescribed, give it, call and tell the family what we did.”[193] But, she clarified, “No, we don’t do that.”
The fact that a director of nursing would make this statement is particularly problematic because the job of seeking informed consent is often delegated, legally, nursing staff.[194] The fact that the head of all nursing staff is unfamiliar with any procedure is a bad sign. As CMS explained in response to comments on its proposed revisions to federal regulations, although only the physician or prescribing practitioner prescribes medication, “[n]urses also bear the responsibility for the medications they administer to residents.”[195] Staff at several facilities that have achieved significant reductions in off-label antipsychotic drug use told Human Rights Watch that they require all requests for antipsychotic drug orders to go through the director of nursing.
BACK TO TOP
IV. Inadequate Government Regulation and Enforcement
The US government has a duty to effectively regulate the nursing home industry with a view to protecting the human rights of residents. This responsibility is particularly important because nursing facilities are institutions with almost complete control over all aspects of the lives of residents. Effective regulation and oversight require not only the establishment of an appropriate regulatory framework to protect people from harm, but also effective enforcement of regulatory standards. Voluntary initiatives like the National Partnership to Improve Dementia Care in Nursing Homes are no substitute for the core CMS functions of regulation and enforcement.[196] Our research found that CMS has failed to use the tools at its disposal to ensure adequate protection for residents’ rights.
Inadequate Regulation
Nursing industry officials frequently claim that nursing homes are the second most regulated sector in the US after the nuclear industry.[197] In a letter to the then-US Department of Health and Human Services Secretary Thomas Price, AHCA wrote: “We are already the most regulated profession in the country.”[198] Following the adoption of the Nursing Home Reform Act of 1987, the federal government has established extensive regulations of the nursing facility sector and requires detailed reporting on numerous aspects of facilities’ operations. Nursing facilities’ participation in the Medicare and Medicaid programs—whose payments make up over half of the average facility’s budget—is contingent upon certification and compliance with these regulations.[199]
Despite the depth and breadth of the regulations, which range from emergency preparedness and infection control to prevention of abuse and neglect, crucial shortcomings remain. Our research on the inappropriate use of antipsychotic medications identified the failure to ensure minimum staffing levels necessary for residents to attain their highest practicable wellbeing and the lack of explicit requirements around informed consent (or functionally equivalent legal requirements that are framed in different terms) as key gaps in existing regulations.
Failure to Set Effective Standard to Address Gross Understaffing
The right to health requires governments to ensure that health services are of adequate quality. Gross understaffing and under-training of staff may contribute to the inappropriate use of anti-psychotics. According to one state long-term care ombudsman: “Insufficient CNAs [certified nurse aides] is the crux of the antipsychotics problem.”[200] The federal government has not taken effective steps to tackle this problem.
Instead of requiring facilities to ensure every resident has a minimum number of nursing staff hours per day or staff per number of residents, CMS imposes a more general requirement that staffing be “sufficient” and “competent,” based on the facility’s own annual assessment of residents’ acuity, diagnoses, and care plans.[201] This self-regulation is inadequate, given the continuing prevalence of staff shortages at many facilities.
CMS has recognized the importance of staffing, saying that staff competency and numbers are “critical to quality of care and resident safety,” and that there is “no question that staffing and quality are associated.”[202] Likewise, numerous studies have shown that adequate staffing—sufficient quantity, training, and consistency of staff—is critically important to the quality of care nursing facility residents receive and that inadequate staffing leads to substandard care.[203] Some studies have found that staffing is the best predictor of deficiencies—findings by government inspectors of substantial non-compliance with the law—and of hospitalization rates of residents, which in turn are associated with neglect.[204]
Interviewees with distinct vantage points on nursing home challenges—residents, ombudsmen, nursing staff, and administrators—agreed that adequate staffing was essential. In Illinois, Barbara Jo V. described her experiences with and concerns about inadequate staff in her nursing home, where she has lived for ten years: “I need help to get to the bathroom. I can’t go by myself. That’s the problem with me. There’s no nurses at night at the station. Think if we had a fire.”[205] Joyce M., another resident of the same facility, where she has lived for five years, said: “You should never wait ten minutes when we have the call light on. I’ve waited an hour for it to be answered. They’re always short of help.”[206] In Kansas, Marisa N., who has lived in several nursing facilities since falling in 2014, said:
I don’t think there’s enough staff. Many of the residents are two-person transfers. I tell you, it’s been very frustrating to me to sit here [in the bathroom] waiting. On weekends it has been horrendous. If they know State [inspectors] is coming, they’ll get six or seven more [staff] than usual to come in. Otherwise it’s just kitchen, waiter, two or three CNAs [certified nurse aides] on the floor, and a nurse.[207]
One former ombudsman in Kansas said: “What distinguishes facilities most of all is their staffing. Especially with dementia, you need consistent staffing.”[208] An ombudsman in Florida said:
I wish they could get quality staff who stay. Poor CNAs make a pittance. A nursing home might meet the minimum staffing requirement but still not meet residents’ needs. AHCA [Florida’s regulatory agency, the Agency for Health Care Administration] has okay’ed one CNA for 20 residents. Some residents need a two-person lift![209]
A nurse in Texas who has worked in nursing homes since 1992 said: “It’s very stressful. The hardest is when there’s not enough help. You can’t do your job the way you know you need to do it. You just do the most basic needs.”[210] A nurse elsewhere in Texas said, “Staffing is the biggest problem across the nation. Here, we don’t have many staff on weekends. So there are no showers on Sundays. Then the workload is less.”[211] An administrator in Texas said: “CNAs are the most important…. They’re the heart of the nursing home and nobody cares. The thinking is, ‘we’ll just get another one.’”[212]
Various studies have found that staffing levels and staff training affect the use of antipsychotic medicines, although some did not find a robust association.[213] Studies that examined efforts to reduce antipsychotic drug use found that staffing and staff training were associated with the success of those efforts. One study found that a full-time advanced practice registered nurse at the nursing home led to a drop from almost one in three to one in ten long-stay residents taking the drugs and “achieved no use of antipsychotic medications for residents with a diagnosis of dementia.”[214] Another study concluded that “[n]urses working longer on the ward, with lower education, presented higher barriers to discontinuation of antipsychotics.”[215]
Governmental studies have underscored the importance of minimum staffing standards, too.[216] In 2001, a CMS-funded study concluded that to avoid compromising quality of care, long-stay residents should have 4.85 nursing staff hours per day, and that short-stay residents should have 4.1 hours.[217] A subsequent report in 2004 by the Institute of Medicine, recommended following these same standards and updating minimum requirements to require at least one registered nurse on duty at all times (not just eight hours a day); staffing levels to increase based on resident numbers, consistent with the 2001 CMS report; and setting staffing levels for nurse aides, recognizing that aides “provide the majority of patient care.”[218]
More than a decade later, staffing at many facilities still falls far short of these recommendations. A review of the data in 2017 shows that almost a thousand nursing facilities reported that they were providing less than three hours of staff time to residents per day—almost 40 percent below the recommended level.[219] Human Rights Watch analysis found that state-level averages of total reported nurse staffing hours vary: Illinois and Texas have two of the lowest levels, at 3.80 and 3.83 hours respectively; California and Florida have two of the highest, at 4.63 and 4.59 respectively.
Moreover, CMS has stated that those numbers are likely inflated because nursing facilities tend to over-report their staffing levels.[220] CMS expects the payroll-based staffing data collection, mandated by the Affordable Care Act, to “greatly assist us in re-evaluating” current staffing short-comings because they expect their “understanding of how facilities are staffed … to improve with the collection of payroll-based staffing data.”[221] One study examining the mix of residents in nursing facilities found that actual staffing levels were lower than predicted, given residents’ needs.[222]
Studies also show the importance of having sufficient registered nurses on staff.[223] Yet federal regulations only require one registered nurse to be on duty for eight consecutive hours per day.[224]
In 2016, CMS rejected a minimum staffing level or ratio.[225] First, it stated that facilities are too different for a one-size-fits-all approach—contrary to the position of the 2001 report that holds that the inability to stratify staffing thresholds by case-mix “would in no way invalidate the thresholds that were identified.”[226] Second, it argued that a minimum staffing requirement could have unintended consequences like “staffing to the minimum” or “stifling innovation,” or could “not result in the improved quality and person-centered care [sought].”[227] Third, CMS concluded that it lacked sufficient data for “determining if and what such [staffing] ratios should be.”[228]
Similarly, AHCA wrote to Human Rights Watch regarding its opposition to stronger staffing requirements:
We feel that requiring staffing levels or ratios does not recognize the difference in types and acuity and care needs different individuals and facilities have. A one shoe [sic] fits all approach would not be helpful to assuring high quality care. Also focusing on just staffing levels is misguided. We believe the focus should be on resident outcomes.[229]
LeadingAge, the nonprofit nursing home trade association, reiterated this perspective in response to a letter from Human Rights Watch:
LeadingAge has not supported minimum staffing ratios because they become just that – minimum standards to which many providers focus on. We believe that staffing should be based on the needs and acuity of the residents served and the skills/competency of the staff that care for them. Of particular note, non-profit providers typically have higher staffing ratios than the for-profit nursing homes in a given geographic area.[230]
Yet the bottom line is that the current standard has not succeeded in pushing nursing facilities to raise staffing levels to the desired levels. A new and more robust approach, which may or may not include minimum staffing levels, is needed. If CMS does not want to establish a specific minimum staffing requirement, it should introduce another approach that is more effective at getting nursing facilities and their owners to address understaffing.
However, based on information gleaned from data from some of the states that have introduced minimum staffing levels, there is no clear evidence that stronger staffing levels mandated by law has led to higher quality of care.[231] Human Rights Watch does not take a position on the means that the government employs to ensure sufficient staff to provide the quality of care required by domestic law and human rights standards. However, the current federal regulations are not doing the job.
Inadequate Free and Informed Consent Laws and Regulation
Federal regulations governing nursing facilities certified by Medicare and Medicaid provide for the right “to be fully informed in advance about care and treatment, to be fully informed in advance of any changes in care or treatment that may affect the resident’s well-being, and (except with respect to a resident adjudged incompetent) to participate in planning care and treatment or changes in care and treatment,” as well as the right to refuse treatment.[232]
The regulations do not require nursing facilities to obtain free and informed consent, written or otherwise, from any residents prior to administering antipsychotic or other psychotropic medications. At least half of states also do not require written, informed consent from individuals living in nursing facilities prior to the administration of antipsychotic drugs.[233]
CMS has an obligation to protect the right of people in nursing facilities to informed consent. In practical terms, meeting that obligation should not require a significant legislative or regulatory shift if existing regulations are enforced rigorously. However, given obstacles to doing so, informed consent remains in effect a gap in the regulations.
Current guidance states that:
[Federal regulations require facilities to involve residents, families, and representatives] in discussions about potential approaches to address behaviors and about the potential risks and benefits of a psychopharmacological medication (e.g., FDA black box warnings), the proposed course of treatment, expected duration of use of the medication, use of individualized approaches, plans to evaluate the effects of the treatment, and pertinent alternatives.[234]
CMS guidance states explicitly that “[r]esidents have the right to be informed about their medical condition, care and treatment; they have the right to refuse treatment and the right to participate in the care plan process.”[235] Individuals in nursing facilities also already have a right to “request, refuse, and/or discontinue treatment.”[236]
Substantively, these requirements would amount to informed consent if the provisions were enforced in practice. However, it is difficult to be sure that adequate information was conveyed in an intelligible fashion and that the person receiving care had the opportunity to make an informed decision about their treatment options.
Existing nursing home regulations already require residents be present for and included as much as possible in discussions and decisions. As dementia is a progressive, degenerative disease, nursing facilities should plan ahead for future situations when a resident may increasingly struggle to make informed decisions about their care. Residents should be proactively engaged to determine their wishes regarding future care in a range of possible scenarios in case it becomes impossible for them to engage in those discussions in the future. It is essential that this planning starts at the point of admission to the facility.
In California, a treating physician may determine that an individual lacks the ability to consent to medical treatment. If there is no legal representative to make the decision on the person’s behalf, California law mandates that the person’s nursing facility convene an interdisciplinary team to make decisions.[237] Many states have no established procedures for a nursing home to follow to make a determination for individuals in these circumstances.
For example, the two informed consent statutes in Texas relating to antipsychotic drugs and nursing home residents make no provision for individuals deemed to lack capacity without a proxy.[238] Otherwise, the law provides that no resident may be administered a psychoactive medication without the resident’s consent unless it is an emergency or “the person authorized by law to consent on behalf of the resident has consented.”[239] The law then enumerates when the resident’s or proxy’s consent is valid, such as when it is voluntary; adequate information was provided on which the person could make the decision; the person giving consent was aware the consent could be revoked; and the consent is documented in the clinical record.[240]
US procedural safeguards in the determination of incapacity are much stronger in the context of civil commitment and mental or intellectual disability law.[241] It is worth exploring whether nursing facility residents’ human rights would be better protected if these protections were to apply to them as well, despite the absence of direct state intervention in their institutional placement.
Ineffective Enforcement
Regulatory standards are only as effective as their enforcement. Our research found several significant shortcomings in enforcement of federal regulations, from the underestimation of harm cited to the inadequate deterrent effect of financial sanctions assessed. Despite widespread failure by nursing facilities to comply fully with regulations put in place to protect people living in these institutions, CMS is not using its full authority to force them to improve their performance.
In November 2017, CMS reduced enforcement requirements further, including placing a moratorium on the issuance of financial sanctions for noncompliance with Obama-era regulatory requirements.[242] Previously, industry groups had critiqued even the government’s inadequate enforcement efforts. For example, LeadingAge, the nonprofit trade association, wrote to Human Rights Watch saying:
We [believe] that the current Survey and Certification system is NOT driving quality and excellence, but is one that is focused entirely on enforcement, that it is inconsistent, that it is punitive in nature and creates a defensive environment—not one that supports innovation and excellence.[243]
In a letter to then-US Department of Health and Human Services Secretary Thomas Price, AHCA pointed out that “a punitive approach by survey teams across the country has threatened to shut down even the best operators in our profession.”[244] As the following analysis demonstrates, it is not accurate that typical penalties are at all onerous.
The trade associations do not argue that the government assesses sanctions when noncompliance has not in fact occurred. Instead, their view is that progress toward compliance with non-negotiable, federal, legal requirements (“we have so dramatically improved quality”) merits being “rewarded for our efforts.”[245]
Moreover, most facilities are part of a chain, where the owner has at least two and sometimes hundreds of nursing facilities.[246] But the government does not sufficiently collect and analyze nursing facility data based on ownership or conduct standard enforcement taking ownership into account.[247] The facility is the only “locus of accountability” in the current enforcement system: a notable shortcoming because in many cases, fundamental decisions—about management, operations, revenue allocation, compliance with state and federal quality of care standards, staffing levels, and government reporting—are not made by the administrators of individual facilities but by upper level managers in the corporate structure that owns them.[248] The main enforcement process authorized by law discussed in the following sections—assessing financial, licensing, and other penalties for failure to substantially comply with regulatory requirements—is exclusively focused on individual facilities.[249]
CMS is the main agency to regulate nursing facilities. However, other government agencies have overarching enforcement authority across sectors, such as the US Department of Justice (DOJ).[250] In 2016, the DOJ created Elder Justice Task Forces to penalize nursing facilities for grossly substandard care.[251]
Underestimation of Severity of Harm Caused by Inappropriate Use of Antipsychotic Drugs
Federal regulations provide for regular inspections of all licensed nursing facilities. CMS contracts with state agencies to conduct enforcement of federal and state laws and regulations.[252] Every 15 months at most, state surveyors conduct unannounced inspections to evaluate facilities’ compliance with health and safety regulations.[253] Surveyors use a detailed protocol—the State Operations Manual produced by CMS, which includes detailed investigative protocols on particular subjects—to conduct surveys and determine the scope and severity of a deficiency.[254] Deficiencies are determinations of noncompliance with more than 150 federal regulatory quality of care, quality of life, safety, fire, and other standards, from freedom from abuse, neglect, and exploitation to the physical environment, emergency preparedness, infection control, food services, and more.[255]
Surveyors identify and substantiate any deficiencies, and then determine the scope and severity of harm. Inspectors determine whether the deficiency is isolated, part of a pattern, or widespread and its consequence: the potential for or actual occurrence of minimal harm, actual harm, or immediate jeopardy (likelihood or occurrence of “serious injury, harm, impairment, or death to a resident”).[256] Table 1 shows the scope/severity grid that surveyors use.
| Deficiency Severity |
Deficiency Scope |
|
Isolated |
Pattern |
Widespread |
| Level 4 — Actual or potential for death or serious injury (immediate jeopardy) |
J |
K |
L |
| Level 3 — Actual harm that is not immediate
jeopardy |
G |
H |
I |
| Level 2 — No actual harm with potential for more than minimal harm |
D |
E |
F |
| Level 1 — No actual harm with potential for
minimal harm |
A |
B |
C |
Table 1. Severity and Scope Grid for Deficiencies
Guidance to surveyors has made clear that an immediate jeopardy citation may be appropriate without any actual harm having yet occurred, that serious harm can result from neglect, and that psychological harm is just as serious as physical harm.[257] Triggers for immediate jeopardy citations include adverse medication consequences and use of chemical restraints without adequate monitoring.[258] Human Rights Watch analysis found that 12 percent of facilities were cited for at least one immediate jeopardy citation between 2014 and 2016; 40 percent of facilities were cited for at least one “actual harm” level deficiency. Every facility was cited for at least one deficiency of some severity level.
CMS guidance for surveyors suggests that many cases of inappropriate use of antipsychotic medications should be tagged as Level 3 or 4 severity. For example, the manual defines a Level 3 deficiency as “clinical compromise, decline, or the resident’s inability to maintain and/or reach his/her highest practicable well-being.”[259] It cites, among others, the following example:
Facility failure to implement a GDR [gradual dose reduction] that was not contraindicated in a resident receiving prolonged, continuous antipsychotic therapy resulting in functional decline, somnolence, lethargy, tremors, increased falling, or impaired ambulation.[260]
Level 4 deficiencies are defined as regulatory noncompliance that:
[H]as allowed, caused, or resulted in, or is likely to allow, cause, or result in serious injury, harm, impairment, or death to a resident; and requires immediate correction, as the facility either created the situation or allowed the situation to continue by failing to implement preventative or corrective measures.[261]
The guidance includes the following examples related to antipsychotic drugs: “Failure to recognize that continuation of an antipsychotic…, has caused significant changes in the resident’s behavior;” “continuation of the antipsychotic without indication resulted in significant psychosocial harm;” and “failure to re-evaluate continuation of an antipsychotic originally prescribed for acute delirium which resulted in significant side effects from the medication.”
Yet Human Rights Watch’s data analysis suggests that deficiencies related to antipsychotic drugs are almost exclusively assessed as “no actual harm.” Our review of more than 7,000 deficiency reports related to antipsychotic drugs between January 1, 2014, and June 30, 2017, found that 97 percent of these deficiencies were tagged as Level 2 (D, E, and F categories), or “no actual harm.” Only 93 deficiencies (1 percent) were tagged as Level 3 (G and H) and 63 deficiencies (less than 1 percent) as Level 4 (J, K, and L). See Table 2 for the distribution of assessed scope and severity. A detailed description of the data analysis performed can be found in Appendix 4.
| Deficiency Severity |
Scope |
Number |
Percent |
Cumulative Percent |
| Level 1 |
B |
5 |
0% |
0% |
| Level 2 |
D |
4,516 |
64% |
64% |
| E |
2,326 |
33% |
97% |
| F |
36 |
1% |
98% |
| Level 3 |
G |
82 |
1% |
99% |
| H |
11 |
0% |
99% |
| Level 4 |
J |
24 |
0% |
99% |
| K |
25 |
0% |
99% |
| L |
14 |
0% |
99% |
|
Total |
7,039 |
|
|
Table 2. Scope and Severity of Drug-Related Deficiency Citations with Antipsychotic Drug-Related Key Terms[262]
A study by the Center for Medicare Advocacy, a national nonprofit, nonpartisan law organization focused on protecting older people’s and people with disabilities’ fair access to Medicare and quality health care, and Dean Lerner Consulting, an attorney consultant with expertise in the long-term care industry, of all deficiency citations for unnecessary drugs (f-tag 329) in 2010 and 2011 from seven states (Georgia, Illinois, Massachusetts, Oregon, Pennsylvania, and Texas) reached a similar conclusion. Of 602 citations, 292 concerned antipsychotic drugs. Almost all—95 percent—were cited at the “no actual harm” level.[263]Examples of what surveyors considered to be “no actual harm” included: a person falling 20 times; becoming more agitated with the drugs; being given more than the “daily recommended dosage;” being prescribed antipsychotic drugs without appropriate evaluation; declining to the point of needing total care; requiring hospitalization for undiagnosed underlying infections; and “spending all her time in bed.”[264]
This apparently systematic underestimation of the severity of harm caused by inappropriate uses of antipsychotic drugs (among other drugs and medical interventions) not only appears to point to woefully inadequate enforcement and protection of nursing home residents’ rights, but also leads to inappropriately light penalties. Without a finding of more severe harm, financial penalties are minimal, optional, or do not attach.[265] A concerted effort from CMS to address this problem is urgently required.
The revised CMS State Operations Manual, which was meant to go into effect on November 28, 2017, before a moratorium on enforcement of significant portions of it was established on November 24, 2017, may go some way toward addressing this routine underestimation of the harm of deficiencies related to antipsychotic drugs if it were enforced.[266] The manual states explicitly that Level 1 deficiencies—for no harm with potential for minimal harm—“does not apply for this regulatory requirement [regarding psychotropic drugs] because the failure of the facility to provide appropriate care and services to manage the resident’s medication regimen to avoid unnecessary medications and minimize negative outcome places residents at risk for more than minimal harm.”[267]
It also provides as an example of a Level 4 deficiency:
Failure to recognize that use of an antipsychotic medication, originally prescribed for agitation, has caused significant changes in the resident’s quality of life. The resident no longer participates in activities that they previously enjoyed, has difficulty concentrating and carrying on conversations, and spends most of the day isolated in his or her room, sleeping in a recliner or in bed. Use of the antipsychotic medication without an adequate clinical indication, GDR attempts, and non-pharmacological approaches resulted in psychosocial harm.[268]
Weak Deterrent Effect of Citations and Penalties in a Remedial Enforcement System
Until they get a tag that bites them, nothing will change. In this industry, there is a real cost-benefit analysis. If the fine will be $100,000, then they’ll hire the three nurse aides who will cost them about the same amount.
—Long-term care consultant in Kansas, January 2017[269]
Appropriate financial sanctions and other penalties for violations of regulatory standards are a critical element of a robust enforcement mechanism. Penalties should be commensurate to the seriousness and nature of the infraction and should seek to bring about enduring changes in practice. While the framework for a meaningful enforcement system exists, our research found that CMS and its state counterparts often impose penalties for serious infractions that are so low, automatically reduced, or negotiable that they do not generate meaningful pressure to address the root causes of violations.[270]
The scope and severity of harm determines the range of potential fines or civil money penalties. Consequences for facilities’ noncompliance with the law fall into three categories. The first category of lightest penalties includes: directed plan of correction; state monitoring; and directed in-service training.[271] In other words, facilities suffer no financial sanction. The only consequence for noncompliance for the lowest scope and severity deficiencies is making a plan to correct the problem.
The second category of penalties includes: denial of payment for all Medicare and/or Medicaid residents; denial of payment for all new admissions; and the lower range of civil money penalties (CMPs), financial sanctions.[272] These penalties, if imposed, may generate financial pressure that incentivizes facilities to take seriously the problem and correct it in a lasting way.
The third category of heaviest penalties includes: termination of the provider agreement; temporary management; and the upper range of CMPs.[273] This category of remedies may include transfer of residents or transfer of residents and closure of facility, at states’ or CMS’ discretion.[274] Historically, government studies of CMS and state level enforcement have found that lower levels of all types of penalties are used much more frequently than higher levels.[275]
Human Rights Watch quantitative analysis of fines assessed in all states between 2014 and 2016 found that 80 percent were less than $10,000 and 20 percent between $10,000 and $100,000. As of July 2017, a citation that is “no actual harm” with potential for more than minimal harm that is widespread can garner a fine of $405 per day or a per instance fine of $5,000.[276] “Actual harm” citations (Levels G, H, and I, depending on scope) can garner a fine between $505 and $2,055 per day and between $10,000 and $15,000 per instance, depending on scope. “Immediate jeopardy” level citations (Levels J, K, and L, depending on scope) can garner a fine between $6,394 and $10,494 per day or between $10,000 and $20,000 per instance, depending on scope. Only the highest level deficiency is now eligible for the top civil money penalties.[277]
Until July 2017, when CMS revised its Civil Money Penalty Tool through sub-regulatory guidance that had no public notice and comment period, CMS Regional Offices were in most cases instructed to impose a per day (that the noncompliance persisted) penalty.[278]Generally, per day penalties are more significant.[279] The Bipartisan Budget Act of 2015 amended the Federal Civil Penalties Inflation Adjustment Act of 1990 to allow the civil money penalty amounts set in 1987 to be adjusted for inflation for the first time.[280]
AHCA pushed for such reductions in March 2017.
Any violation in the SNF [skilled nursing facility] setting, no matter how small, is treated as a violation of the requirements of participation in Medicare and Medicaid and puts the SNF on a termination track from these programs. These violations can also result in large Civil Monetary Penalties (CMPs)…. The use of CMP’s is out of control…. We have seen a dramatic increase in CMPs being retroactively issued and used as a punishment.[281]
The sub-regulatory guidance appears to respond to some of AHCA’s specific requests.
Analysis of data on deficiencies related to antipsychotic drugs and rates of use of these medicines by nursing facilities, however, suggests that the issuance of deficiency citations without financial sanctions attached—the current situation given routine practice of assessing antipsychotic drug-related deficiencies as Level 2, with corresponding lighter penalties—has little impact on the off-label use of these medications, raising concerns about the deterrent effect of current enforcement.
To assess the impact of antipsychotic drug-related deficiency citations, we compared rates of antipsychotic drug use in people without an exclusionary diagnosis for the 4,221 unique facilities that received a cumulative 5,880 antipsychotic related deficiencies.[282] In the year following an antipsychotic drug-related deficiency citation, facilities reduced their antipsychotic drug use rate in people without an exclusionary diagnosis by 1.5 percentage points (see Table 3).
| Citation year |
Number of citations |
Average percentage point change |
| 2014 |
1,118 |
-0.55 |
| 2015 |
1,749 |
-2.43 |
| Q1 2016 |
493 |
-1.02 |
Table 3. Change in Antipsychotic Drug Use in People without an Exclusionary Diagnosis in the Year Following an Antipsychotic Drug-Related Citation
EXPAND
Graph 1. Antipsychotic Related Citations Have Minimal Effect on Antipsychotic Use Rates
However, there was no statistically significant difference in the rate of change in antipsychotic drug use between facilities that received an antipsychotic deficiency citation and those that did not.[283] Facilities reduced their antipsychotic drug use by 1.57 percentage points on average in the year following a citation, but those same facilities were already reducing their rates by 1.60 percentage points during periods where they were not cited, and facilities that were not cited at all were reducing their rates by 1.29 percentage points. Between 2014 and the first quarter of 2016, the average reduction in antipsychotic use rates was only 0.031 percentage points greater in facilities that received an antipsychotic related citation compared with those that were not cited. For detail on the statistical analysis performed, see Appendix 4.
| Efforts to Reduce Inappropriate Use of Antipsychotic Medicines
Since 2012, the national antipsychotic drug rate among people in nursing facilities who do not have schizophrenia, Huntington’s disease, or Tourette syndrome, and most of whom have dementia, has declined from 24 percent in 2011 to 16 percent at the end of 2016.[284] (Appendix 3 provides a graph of state reductions between 2011 and 2016.) This decline corresponds to the period since CMS established the National Partnership to Improve Dementia Care in Nursing Homes, in response to significant public and Congressional pressure to address the pervasive and dangerous excessive use of antipsychotic drugs.[285] As no thorough evaluations have been conducted of the Partnership, it is not clear to what extent or through what mechanisms the Partnership contributed to this decline.
The Partnership sought to reduce the rate of antipsychotic drug use in nursing facilities as one way to “enhance the quality of life for people with dementia [and] protect them from substandard care and promote goal-directed, person-centered care for every nursing home resident.”[286]
The initiative primarily set voluntary targets for the industry to attempt to reduce the number of people given antipsychotic medications in violation of their rights and of federal and state regulatory requirements. Since 2016, CMS has not set any new targets for reduction. It provided educational and training materials and opportunities to help the industry attain such reduction. The initiative did not focus on informed consent.[287]
Human Rights Watch visited a number of facilities that significantly reduced levels of antipsychotic drug use in the last year. In each case, the facility had either experienced corporate pressure to reduce the percent of residents on the drug or had an administrator or director of nursing who had taken it upon him or herself to insist on the reduction—including if that meant challenging a doctor or family member. The increased industry-wide attention to the issue and having a central figure within a facility manage the reduction appeared to be critical elements of the reductions. |
Binding Arbitration Agreements
In many contexts, individuals use civil tort lawsuits to secure accountability and redress for abuses the law does not otherwise prevent or punish. Approximately half of the country’s nursing facilities ask residents (or their proxies) to sign binding arbitration agreements upon admission; some make it a condition of admission.[288] Under these contract clauses, disputes between the facility and resident must be resolved outside of the court system. In other words, the resident “waiv[es] his or her right to judicial relief for any potential cause of action covered by the agreement.”[289] Instead, disputes that may arise are resolved through arbitration proceedings. As is true in many other contexts, these agreements raise concerns about whether arbitration offers a fair and impartial hearing and a realistic chance at remedy.
In 2016, CMS banned the use of pre-dispute arbitration clauses, describing them as “fundamentally unfair” because “it is almost impossible for residents or their decision-makers to give fully informed and voluntary consent to arbitration before a dispute has arisen.”[290] Instead of limiting avenues for relief in cases of violations “residents should have a right to access the court system if a dispute with a facility arises.”[291]
CMS noted that “there is significant evidence that pre-dispute arbitration agreements have a deleterious impact on the quality of care for Medicare and Medicaid patients” in nursing facilities.[292] It also emphasized that while arbitration proceedings are widespread in the healthcare industry, the “significant differential in bargaining power” between residents and nursing facilities—the former depends on the latter for almost all their needs—make it “unconscionable” for such facilities to demand, as a condition of admission, that residents sign a pre-dispute agreement for binding arbitration.
In June 2017, CMS did a complete about-face, issuing a new proposed rule that not only would eliminate provisions prohibiting pre-dispute arbitration, but also would allow facilities to deny admission to a resident who refuses to sign the arbitration agreement.[293]
In justifying its reversal, CMS stated that the binding contracts are “advantageous to both providers and beneficiaries because they allow for the expeditious resolution of claims without the costs and expense of litigation,” adding that “this proposal is consistent with our approach to eliminating unnecessary burden on providers, and supports the resident’s right to make informed choices about important aspects of his or her healthcare.”[294]
Proposed federal tort reform legislation could pose additional obstacles to obtaining a remedy for harm. At time of writing, the House of Representatives had passed and the Senate had received H.R. 1215, the Protecting Access to Care Act of 2017, which would impose a three-year statute of limitations for individuals to sue nursing homes for harm, a $250,000 cap on damages, and a limit on attorney contingency fees.[295]
These measures would likely not only reduce the compensation an individual might receive for serious harm or wrongful death, but also deter lawyers from taking the cases in the first place. Other proposals would limit class action lawsuits and the number of years after a harm occurs that a plaintiff could sue, whatever occurred—abuse, neglect, sexual assault—by a number of providers of medical care, including nursing facilities.[296]
BACK TO TOP
V. International Human Rights and US Law
Key Obligations Arising from International Human Rights Law
Torture and Other Cruel, Inhuman, and Degrading Treatment
The Convention on the Rights of People with Disabilities (CRPD), which the US has signed but not ratified, requires governments to “take all effective legislative, administrative, judicial or other measures to prevent persons with disabilities, on an equal basis with others, from being subjected to torture or cruel, inhuman or degrading treatment or punishment.”[297] The US is not legally bound by the CRPD, but the Convention does represent an important authority on the measures the government should take to protect and improve respect for the rights of people with disabilities.[298]
In 2013, Juan Mendez, then the UN special rapporteur on torture and other cruel, inhuman or degrading treatment or punishment, warned of the danger of human rights violations in the healthcare setting where the perception persists that “certain practices in health-care may be defended by the authorities on grounds of administrative efficiency, behaviour modification or medical necessity.”[299]
Mendez also noted that “medical treatments of an intrusive and irreversible nature, when lacking a therapeutic purpose, may constitute torture or ill-treatment when enforced or administered without the free and informed consent of the person concerned.” He also emphasized that an act may constitute ill-treatment, even if it is “intended to benefit the ‘patient’” and may “exist alongside ostensibly therapeutic aims.”
Mendez stated that this rights violation is particularly likely to occur when the “treatments are performed on patients from marginalized groups, such as persons with disabilities, notwithstanding claims of good intentions or medical necessity.”[300] The use of a “prolonged restraint” may constitute torture and ill-treatment; when used against people with mental disabilities, “even a short period of time may constitute torture and ill-treatment.”[301]
The Right to Health and Informed Consent
The highest attainable standard of physical and mental health is a fundamental human right enshrined in numerous international human rights instruments, including the Universal Declaration of Human Rights, the International Covenant on Economic, Social, and Cultural Rights, and the CRPD. The special rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health has expressed that informed consent “is a core element of the right to health, both as a freedom and an integral safeguard to its enjoyment.”[302]
In the words of the special rapporteur on the right to health:
Informed consent is not mere acceptance of a medical intervention, but a voluntary and sufficiently informed decision, protecting the right of the patient to be involved in medical decision-making, and assigning associated duties and obligations to health-care providers. Its ethical and legal normative justifications stem from its promotion of patient autonomy, self-determination, bodily integrity and well-being.[303]
Informed consent is fundamental to “respecting an individual’s autonomy, self-determination and human dignity.”[304]
The special rapporteur on the right to health called on States to:
[R]adically reduce medical coercion…, [and] not to permit substitute decision-makers to provide consent on behalf of persons with disabilities on decisions that concern their physical or mental integrity; instead, support should be provided at all times for them to make decisions, including in emergency and crisis situations.[305]
However, the special rapporteur acknowledged that such change “is a challenging process that will take time” and emphasized the importance of taking intermediary steps:
- Mainstream alternatives to coercion in policy with a view to legal reform;
- Develop a well-stocked basket of non-coercive alternatives in practice;
- Develop a road map to radically reduce coercive medical practices, with a view to their elimination, with the participation of diverse stakeholders, including rights holders;
- Establish an exchange of good practices between and within countries;
- Scale up research investment and quantitative and qualitative data collection to monitor progress towards these goals.[306]
Key Domestic Legal Protections
US federal and state laws protect against abuse and neglect in skilled nursing facilities, primarily through the Nursing Home Reform Act of 1987 and associated regulations.[307]Some of these protections on the quality of care and quality of life a person is entitled to receive while living in a nursing facility are listed explicitly as “resident rights.”[308] Many enumerated rights pertain to antipsychotic medications, discussed below; they also provide for the context of broader care planning based on every individual’s goals and preferences.
These latter rights include: the facility’s promotion of residents’ dignity; the provision of activities to meet individual needs; the provision of medically-related social services; resident assessments as the foundation for all care comprehensive care planning that involves the resident; professional quality services; availability of psychosocial services; sufficient nursing staff; care supervised by a physician; pharmacist reviews of drug regimens; effective administration of facilities; competence of nursing staff; and facilities’ supervision by a medical director.[309]
Other federal and state laws address the protection of people’s rights when living in a nursing facility. Federal laws include the Americans with Disabilities Act, since anyone eligible to live in a nursing facility meets the definition of having a disability, and the Civil Rights of Institutionalized Persons Act, though only for the minority of individuals living in publicly-owned nursing facilities.[310] State laws concerning nursing facilities’ regulation and residents’ rights generally emulate the federal law while setting out distinct provisions on some issues that nonetheless comply with federal minimum standards.
Freedom from Chemical Restraints, a Form of Abuse, and Unnecessary Drugs
Federal and state laws protect individuals in nursing facilities from chemical restraints and other forms of abuse. US regulations also prohibit the use of any unnecessary drugs, including antipsychotic drugs, in nursing facilities even if they do not amount to chemical restraints.[311]
Regulations particular to psychotropic drugs mandate that any prescription for someone not already taking such medication must be “necessary to treat a specific condition as diagnosed and documented in the clinical record”; and anyone given psychotropic medications must “receive gradual dose reductions, and behavioral interventions, unless clinically contraindicated, in an effort to discontinue these drugs.”[312] For antipsychotic drugs, gradual dose reduction must be attempted twice in the first year of administration and annually thereafter.[313]
Informed Consent and Right to Refuse Treatment
The Nursing Home Reform Act does not provide for express, written informed consent. However, it provides for the right to be fully informed of one’s health status; the right to participate in treatment planning; the “right to be informed in advance, by the physician or other practitioner or professional, of the risks and benefits of proposed care, of treatment and treatment alternatives or treatment options and to choose the alternative or option he or she prefers”; and the right to refuse treatment.[314]
Most state laws do not expressly require written informed consent prior to the administration of antipsychotic drugs to individuals in nursing facilities.[315] However, some state laws do, and in all states, this right should be protected by a combination of nursing home laws and state civil tort statutes. Texas, California, and Illinois are examples of states that require informed consent explicitly, although without a private right of action as a basis to sue if this right is violated. The Texas Health & Safety Code provides for the right to “refuse to consent to the prescription of psychoactive medications;” sets out the requirements for informed consent, including its voluntary and revocable nature and the information that must be provided, and its documentation; and establishes the limited circumstances where it is not required.[316]
California’s Patients’ Rights article states: “Patients shall have the right … to consent to or to refuse any treatment or procedure,” including to receive all relevant information for making the decision.[317] For psychotherapeutic drugs specifically, the informed consent discussion must include the reason for the treatment, nature of the intervention including the duration, likely benefit with and without treatment, side effects and risks, reasonable alternatives, and the patient’s right to accept, refuse, and revoke consent.[318]
Illinois’s Nursing Home Reform Law provides that psychotropic medication, including antipsychotic drugs, “shall not be prescribed without the informed consent of the resident, the resident’s guardian, or other authorized representative.”[319] Informed consent requires a discussion between the individual concerned or his or her representative and the physician, pharmacist, or nurse regarding the “possible risks and benefits of a recommended medication,” documented in a standard fashion.[320]
New York and Florida are examples of states with laws that expressly mimic the federal law. New York’s statute provides that individuals in nursing facilities have the right to “be fully informed of his or her medical condition and proposed treatment…, and to refuse medication and treatment after being fully informed of and understanding the consequences of such actions.”[321]
Florida’s statute provides for nursing home residents’ right to “be adequately informed of his or her medical condition and proposed treatment,” the right to “be fully informed in advance of any nonemergency changes in care or treatment,” and the right to “participate in the planning of all medical treatment, including the right to refuse medication and treatment.”[322]
Kansas is an example of a state that does not require informed consent. Its administrative regulations for all adult care homes, including nursing facilities, provide for the right to “refuse treatment” only.[323] Kansas and states like it are bound by federal requirements.
Americans with Disabilities Act
Based on the admission criteria for skilled nursing facilities and nursing facilities, almost all nursing facility residents are protected by the Americans with Disabilities Act (ADA) of 1990.[324] The ADA defines disability as: “a physical or mental impairment that substantially limits one or more major life activities” or “a record of such an impairment.”[325] A disability under this law could also be merely “being regarded as having such an impairment … whether or not the impairment limits or is perceived to limit a major life activity,” so long as the impairment is not “transitory” (lasting six months maximum) or “minor.”[326]
The US Attorney General has jurisdiction to enforce the ADA: to prosecute the violation of the rights of people with disabilities articulated under it. However, it does not have exclusive jurisdiction; private individuals may sue as well. Anyone who has been “subjected to discrimination on the basis of disability … may institute a civil action for preventive relief, including an application for a permanent or temporary injunction, restraining order, or other order.”[327] The ADA has not been employed frequently to protect the rights of older people in nursing facilities. However, it is a relevant legal protection for people with dementia.
BACK TO TOP
Recommendations
To the Centers for Medicare & Medicaid Services
- Strengthen enforcement of existing regulatory requirements in conjunction with contracted state agencies to end all inappropriate use of antipsychotic medication in nursing facilities, including when the medication would be an “unnecessary drug;” when it would amount to a chemical restraint; when it would be inconsistent with other regulatory requirements; and when it is not based on free and informed consent (or functionally equivalent legal requirements that are framed in different terms).
To the United States Congress
- Reintroduce and pass S. 3604, “Improving Dementia Care Treatment for Older Adults Act of 2012,” to amend Title XVIII and Title XIX of the Social Security Act to require standardized protocol for obtaining written, free, and informed consent from an older person with dementia prior to prescribing an antipsychotic drug or from the person’s representative as appropriate.
- Reintroduce and pass H.R. 952, “Put a Registered Nurse in the Nursing Home Act of 2015,” to amend Title XVIII and Title XIX of the Social Security Act to require nursing facilities to use the services of at least one registered professional nurse 24 hours a day, seven days a week, to provide assessment, surveillance, and direct care to residents.
Until the inappropriate use of antipsychotic medications in older people with dementia in nursing facilities ceases completely, the following entities should take interim steps to contribute to the drastic and immediate reduction in inappropriate, sometimes coercive, and irreversibly harmful, uses of the medications:
To the Federal Government
To the Centers for Medicare & Medicaid Services
For Free and Informed Consent:
- To the greatest extent of its authority, require free and informed consent from the individual whose care is concerned, including with support as needed in the decision, or their appointed representative, as long as this representative is chosen freely and is tasked with reflecting the individual’s will and preferences.
- Develop and implement models of supported decision-making that enable people living in nursing facilities to make their own decisions about treatment and care.
- Strengthen enforcement of existing regulatory requirements related to informed consent, appropriate medication administration, and care planning regulatory provisions, including the rights to refuse treatment; to be involved in care planning; to be free from unnecessary drugs; to be free from chemical restraints, and to receive necessary care to achieve the highest practicable wellbeing.
For Adequate Minimum Staffing:
- Revise the final rule for Requirements for Long-Term Care Facilities for Participation in the Medicare and Medicaid Programs to require a 24/7 registered nurse presence, and to establish stronger minimum nurse staffing levels or ratios or other stronger and more enforceable minimum requirements to provide care compliant with the law.
- Publish payroll-based staffing data, as required by the Affordable Care Act, without delay and audit the Payroll-Based Journal submission system.
- Consider automatic penalties to facilities that do not meet minimum quantitative and qualitative staffing requirements, such as imposing a temporary ban on the entrance of new residents until staffing numbers are in compliance with the law.
For Enforcement Efforts Specific to Antipsychotic Medications:
- Strengthen enforcement of existing requirements around unnecessary drugs, chemical restraints, and all other relevant resident rights.
- Amend deficiency categorization guidance for antipsychotic medication-related deficiencies. Inappropriate uses of antipsychotic medications should automatically be considered a Level 3 or 4 severity level unless there is a basis to lower it.
- Amend the Psychosocial Outcome Severity Guide and Investigative Protocol to take into account the particular risks of antipsychotic medications in people with dementia. The Investigative Protocol should provide concrete examples of the occasions when the inappropriate use of antipsychotic drugs would not amount to a Level 3 or 4 severity level.
- Create a discrete f-tag, the identifier for each health or safety issue within the federal regulations for which facilities may be cited for noncompliance, for inappropriate uses of antipsychotic medications. Currently, the deficiency citations for chemical restraints, unnecessary drugs, right to refuse treatment, and other relevant citations do not distinguish between any types of treatment or drugs.
- Consider creating a new survey protocol for any facility with a high antipsychotic medication rate that takes into account potential problems of lack of medical necessity and lack of free and informed choice in accepting the medication.
For General Enforcement to Protect Residents’ Rights and Wellbeing:
- Ensure greater compliance with reporting abuse and neglect allegations. Per US Department of Health and Human Services Office of Inspector General recommendations, improve mechanisms to reduce underreporting of abuse and neglect.
- Retract the July 7, 2017, sub-regulatory guidance to state survey agency directors revising the Civil Money Penalty Tool, which reduces potential dollar amounts of penalties assessed for many instances of substantial noncompliance, and the November 24, 2017, 18-month moratorium on enforcement of critical regulatory requirements.
- Collect, analyze, make publicly available, and conduct enforcement based on ownership-level data to the greatest degree of its authority. Disseminate ownership-level data for oversight and enforcement purposes among federal and state governmental agencies.
To the US Department of Justice
For Enforcement Efforts Specific to Antipsychotic Medications, and for General Enforcement to Protect Residents’ Rights and Wellbeing:
- Increase investigation and enforcement of nursing facilities, nursing facility chains, pharmaceutical companies, and individual pharmacists and providers under the Americans with Disabilities Act; Civil Rights of Institutionalized Persons Act; False Claims Act; and Food, Drug, and Cosmetic Act, among other legal bases of authority.
- Increase attention to inappropriate and nonconsensual uses of antipsychotic drugs within the Elder Justice Initiative efforts to combat the delivery of grossly substandard care.
- Expand efforts of the Elder Justice Task Forces beyond the first 10 regions to improve cooperation among more states’ US attorneys’ offices, state Medicaid fraud control units, state and local prosecutors’ offices, the US Department of Health and Human Services, state adult protective services agencies, state long-term care ombudsman programs, and law enforcement to protect the rights of all individuals in nursing facilities.
To State Governments
To State Legislatures
For Free and Informed Consent:
- Pass legislation to require written, free, and informed consent prior to the administration of antipsychotic medications to individuals in state-licensed nursing facilities, ensuring that the violation of this right is actionable under state law by providing a private right of action and that individuals in need of support for decision-making are afforded it.
- Expand supported decision-making measures and amend relevant statutes to require that supported decision-making processes and supports be available and used as appropriate for people who need support to exercise their right to free and informed consent.
- Take steps to minimize and ultimately reduce to zero the number of individuals in nursing facilities who are deprived of their legal capacity, formally or informally, requiring outreach where appropriate to those who know the individual and can assist, formally or informally, with decision-making.
- Pass legislation to ensure that an individual’s treating physician is not the same person authorized to make a capacity determination and determine subsequent treatment.
For Adequate Minimum Staffing:
- Pass legislation establishing stronger minimum nurse staffing levels and qualifications. Alternatively, pursue other measures to ensure staffing is adequate to provide all residents with necessary care to achieve their highest practicable wellbeing.
For Enforcement Specific to Antipsychotic Medications:
- Eliminate statutory provisions that curtail enforcement for lower level citations.
- Pass legislation to require nursing facilities to adopt, implement, and enforce a policy requiring any employee providing direct care to an individual with Alzheimer’s disease or other forms of dementia to complete a training on providing care to meet their needs.
For General Enforcement to Protect Residents’ Rights and Wellbeing:
- Pass legislation to require more significant state civil money penalties and fines instead of adhering to the federal minimum ranges, with a focus on abuse and neglect.
To State Attorneys General Offices, State Departments on Aging, Disability, Elder Affairs, and Public Health, and Other State Agencies
For Free and Informed Consent:
- Provide resources to assist nursing facilities to connect residents with supported decision-making resources, and require nursing facilities to post this information inside facilities, as it does with long-term care ombudsman services posters.
- Take measures to maximize the use of advanced directives, living wills, and, as appropriate, proxies or surrogates.
- Conduct public service message campaigns to ensure that individuals know that they have the right to informed consent, including with regard to the administration of antipsychotic drugs and other nonemergency medical interventions.
For Enforcement Specific to Antipsychotic Medications
- Keep track of facilities and chains using antipsychotic drugs at higher than average rates or struggling to reduce their rate of use to provide additional oversight, or take other appropriate action to protect the rights of residents at heightened risk of nonconsensual and inappropriate uses of antipsychotic drugs.
For General Enforcement to Protect Residents’ Rights and Wellbeing:
- Require Medicaid fraud control units to investigate and prosecute abuse, including the use of chemical restraints, and neglect in nursing facilities.
To State Long-Term Care Ombudsman Programs
For Enforcement Specific to Antipsychotic Medications:
- Ensure that in facilities with significant percentages of residents receiving antipsychotic drugs without an exclusionary diagnosis and in facilities where individuals appear at risk of being given antipsychotic drugs without their consent or as chemical restraints, volunteer and staff ombudsmen provide general information to all residents, families, and staff regarding the right to be fully informed about treatment; the right to refuse treatment; and the right to informed consent in states that provide for it. Consider disseminating publicity information produced by CMS, advocacy organizations, AHCA, and others on antipsychotic drugs in people with dementia.
For General Enforcement to Protect Residents’ Rights and Wellbeing:
- Fulfill obligation under Older Americans Act to “analyze, comment on, and monitor the development and implementation” of all local, state, and federal law, regulation, policy and actions pertaining to residents’ rights; recommend appropriate changes; facilitate public comment; and “provide leadership to statewide systems advocacy efforts … on behalf of long-term care facility residents.”
- Ensure regional, staff, and volunteer ombudsmen understand that their mandate and responsibility under the Older Americans Act is not to mediate disputes between residents and nursing facilities but to “represent the interests of residents before governmental agencies” and ensure residents’ access to “administrative, legal, and other remedies to protect the health, safety, welfare, and rights of residents.”
BACK TO TOP
Acknowledgments
This report was researched and written by Hannah Flamm, New York University School of Law Fellow at Human Rights Watch’s Health and Human Rights Division. Megan McLemore, senior researcher in the Health and Human Rights Division; Bethany Brown, researcher in the Health and Human Rights Division; and Diederik Lohman, director of the Health and Human Rights Division provided additional research support. Brian Root, quantitative analyst in the Program Office, provided quantitative data analysis. Josh Lyons, satellite imagery analyst in the Program Division, provided geospatial analysis.
The report was edited by Diederik Lohman; Chris Albin-Lackey, senior legal advisor; and Babatunde Olugboji, deputy program director. The report was reviewed by Emina Cerimovic, researcher in the Disability Rights Division; Arvind Ganesan, director of the Business and Human Rights Division; and Allison Parker, co-director of the United States Program.
Matthew Parsons, associate in the Health and Human Rights Division, provided production assistance and support. Layout and production were done by Rebecca Rom-Frank, photo and publications coordinator; Jose Martinez, senior coordinator; and Fitzroy Hepkins, production manager. Erinma Kalu, Grace Neumann, Delphine Spitaels, Courtney Tran, Romsin Zaya, and Jing Zhao, interns and fellows in the Health and Human Rights Division, provided research support.
This report would not have been possible without the generosity, courage, honesty, and incisiveness of so many people living in nursing facilities, their families and advocates, as well as facility staff. We are grateful to the many advocates, medical professionals, and scholars who greatly enriched the quality and depth of our research, analysis, and reporting. Thank you to Sarah Burger, senior adviser to the Hartford Institute for Geriatric Nursing; Tony Chicotel, senior attorney at California Advocates for Nursing Home Reform; Martha Deaver, president of Arkansas Advocates for Nursing Home Residents; Patty Ducayet, National Association of State Long-Term Care Ombudsman Programs and State Long-Term Care Ombudsman of Texas; Toby Edelman, senior attorney at the Center for Medicare Advocacy; Dr. Jonathan Evans, former president of the American Medical Directors Association; Amanda Fredriksen, associate state director of advocacy for the AARP Texas State Office; Charlene Harrington, professor emeritus at the University of California San Francisco; Jeff Kelly Lowenstein, investigative journalist, author, and professor at Columbia University’s Graduate School of Journalism; Karen Love, executive director of the Dementia Action Alliance; Mitzi McFatrich, executive director of Kansas Advocates for Better Care; Wendy Meltzer, executive director of Illinois Citizens for Better Care; Richard Mollot, executive director of the Long-Term Care Community Coalition; Sam Roe and David Jackson, investigative reporters of the Chicago Tribune; Penny Shaw, member of the board of Massachusetts Advocates for Nursing Home Reform; Lori Smetanka, executive director of the National Consumer Voice for Quality Long-Term Care; Margie Sullivan, executive director of Texas Advocates for Senior Care; Janet Wells, consultant for California Advocates for Nursing Home Reform; and many others including those not identified by name to protect confidentiality.

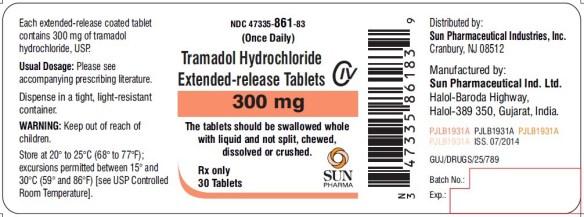








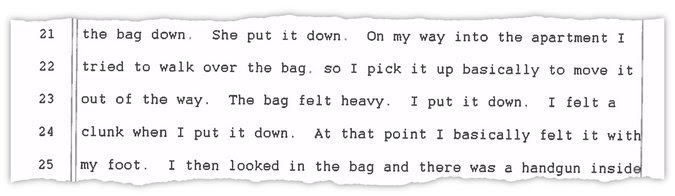








 Eden Gardens Assisted Living Facility was ordered closed by the state.
Eden Gardens Assisted Living Facility was ordered closed by the state.



 Philip Esformes was listed as the owner/manager of Eden Gardens for 11 years. He is now in federal prison.
Philip Esformes was listed as the owner/manager of Eden Gardens for 11 years. He is now in federal prison.
 Photo: Shutterstock
Photo: Shutterstock